Академический Документы
Профессиональный Документы
Культура Документы
Syncope 08.29.2018
Загружено:
Emily Eresuma0 оценок0% нашли этот документ полезным (0 голосов)
272 просмотров16 страницPediatric Morning Report
Оригинальное название
syncope_08.29.2018
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документPediatric Morning Report
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
272 просмотров16 страницSyncope 08.29.2018
Загружено:
Emily EresumaPediatric Morning Report
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 16
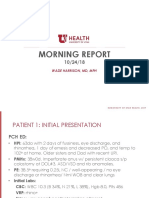
Morning Report Case Presentation
AUGUST 29, 2018
Case: Initial Presentation
CC: Fall, Possible Seizure
HPI:
- Running on sidewalk at school when
she fell
8 y/o previously healthy female
transferred from OSH to PCH ED for - Unconscious per witnesses, initial
fall, possible CHI and seizure. GCS 8 per EMS
- Possible seizure (uncertain timing)
- Seen initially at OSH:
◦ Head CT reportedly normal
◦ Received Zofran for N/V
Case: Differential Diagnosis
- Primary mechanical fall w/ associated injuries
(Concussion, ICH, Skull fracture, post-impact
seizure)
- Primary seizure/neurologic event w/ secondary
fall (?Underlying IC process, Seizure D/O,
intoxication)
- Primary syncopal event
◦ Cardiogenic
◦ Neurologic
◦ Vasovagal
◦ Metabolic
◦ Other
PE: GCS 15, No head injuries noted, CV normal, RESP normal,
NEURO: CN intact, PERRL, Gait normal, Coordination intact
Case:
ED Work-up & CT Head (overread): Normal head CT
Outcome
ECG: NSR, Normal axes and intervals, QTc 411 msec
Patient discharged home with concussion care information
Case:
Re-presentation HPI:
to ED - Running across field when patient fell
forward, unconscious
Approximately 5 weeks later… - Bystander CPR initiated
- Initial GCS 3, irregular respirations
Patient presents to
- Intubated by EMS
PCH ED in cardiac arrest
- CPR/Resus x14 minutes (EMS) with ROSC
following a witnessed (Total down time 24 minutes from collapse)
collapse
while running at school. - Admitted to PICU
Intubated, mechanically ventilated
Required pressor support for decreased function, evidence of
myocardial ischemic injury on ECG
Concern for underlying arrhythmia
Multiple episodes of short runs of VT, sinus tachycardia, and sinus bradycardia Case:
MRI with diffuse ischemic injury PICU Course
-Acutely decompensated 1 week into PICU course; found to have
uncal/transtentorial/tonsillar herniation
Brain death exam x2 on Hospital Day 8
Syncope:
Benign vs.
Dangerous
Benign vs. Dangerous
Syncope: Benign (Non-life threatening)
15-25% of adolescents have 1+ episode of syncope
Vasovagal Syncope (most common)
◦ UNCOMMON before adolescence
◦ Prodrome of dizziness, nausea, pallor, palpitations, headache
◦ Associated with POSITION CHANGES/STANDING
◦ Paradoxical fall in BP and HR
Postural Orthostatic Tachycardia Syndrome (POTS)
◦ Venous pooling associated with standing
◦ Increased HR; Stable/mildly decreased BP
Syncope: Benign and Other Causes
Exercise-related Syncope
◦ Sudden syncope immediately AFTER strenuous activity
◦ Related to venous pooling with cessation of activity + Dehydration
◦ Should warrant work-up to differentiate from pathologic arrhythmias
Other Causes
◦ Hypovolemia
◦ Dysautonomia (deconditioning, medications [CCB, β-blockers, diuretics],
neuropathies)
◦ Hyperventilation (hypocapnia)/Anxiety
◦ Metabolic derangements (ex. Hypoglycemia)
Syncope: Dangerous (Cardiac) Causes
ARRHYTHMIAS STRUCTURAL
◦ Long QT Syndrome ◦ Aortic Stenosis
◦ Short QT Syndrome ◦ Pulmonary Stenosis
◦ WPW ◦ HOCM
◦ Brugada Syndrome ◦ Pulmonary Hypertension
◦ Catecholaminergic ◦ Coronary Artery Anomalies (KD, Anomalous
Polymorphic CA)
Ventricular
Tachycardia (CPVT)
◦ AV Block MYOCARDIAL DYSFUNCTION
◦ Arrhythmogenic RV Dysplasia
◦ Cardiomyopathy
◦ Myocarditis
Syncope Red Flags
- Sitting or recumbent
- Outside typical age or no prior episodes
- DURING exercise
- No prodrome
- Palpitations or racing heart rate prior to syncope
- LOC >1 minute
- Family history of unexplained deaths, arrhythmias, pacemaker/ICD, or unexplained
drownings
- ECG abnormalities
◦ Long/Short QT
◦ Pre-excitation/Delta Waves (WPW)
◦ RBBB + J-point elevation (Brugada)
On INITIAL presentation, what should have prompted further investigation?
- No prior history of syncopal episodes or seizures
- Episode occurred DURING activity
Case in Review - No prodrome
- No evidence of head injury on exam or imaging
(to support seizure secondary to injury)
History, History, History
• * Sensitivity limited for intermittent
ECG arrhythmias (i.e., CPVT, RV dysplasia)
Echocardiogram
• * If exam/history concerning for
structural problem Next Steps
• Cardiology
Consults • Neurology
• Exercise stress test, Ambulatory
Specialty testing monitoring, EP studies
Case Wrap Up
No autopsy performed/No cardiac pathology collected
Suspected underlying arrhythmia
• Most likely CPVT, ARVD, or rare inherited arrhythmia
• Genetic testing sent for inherited arrhythmiasVariant of unknown significance found
Siblings referred to cardiology
• No major ECG abnormalities found
• Will follow periodically for re-evaluation
Resources
Park MK. Park’s Pediatric Cardiology for Practitioners, 6th Ed. Elsevier Saunders. 2014
Cannon B, Wackel P. “Syncope”. Pediatrics in Review. 2016; 37(4): 159-168.
Rizzo C, Monitillo F, Iacoviello M. “12-lead electrocardiogram features of arrhythmic risk: A focus
on early repolarization”. World Journal of Cardiology. 2016; 8(8): 447-455.
Toscano J. “Review of important ECG findings in patients with syncope”. American Journal of
Clinical Medicine. 2012; 9(2): 92-96.
Buxton A, Zimetbaum PJ, Downey BC. “Catecholaminergic polymorphic ventricular tachycardia”.
UpToDate. July 2018.
Вам также может понравиться
- Primary Adrenal InsufficiencyДокумент26 страницPrimary Adrenal InsufficiencyEmily EresumaОценок пока нет
- Morning Report 9/5/18: Adam Cardullo, MD Pgy - 2Документ22 страницыMorning Report 9/5/18: Adam Cardullo, MD Pgy - 2Emily EresumaОценок пока нет
- Limping 12.10.2018Документ32 страницыLimping 12.10.2018Emily Eresuma100% (1)
- Botulism 08.16.2013Документ12 страницBotulism 08.16.2013Emily EresumaОценок пока нет
- Practice Based Learning (Grand Round)Документ48 страницPractice Based Learning (Grand Round)AnnumОценок пока нет
- More Than A Sore ThroatДокумент17 страницMore Than A Sore ThroatEmily EresumaОценок пока нет
- Morning Report: Sarah Todd, PGY-3 August 7, 2015Документ19 страницMorning Report: Sarah Todd, PGY-3 August 7, 2015Emily EresumaОценок пока нет
- MysteryCase 10.22.18Документ10 страницMysteryCase 10.22.18Emily EresumaОценок пока нет
- Pediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Документ35 страницPediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Emily EresumaОценок пока нет
- Bells Palsy or Stroke 02.06.2019Документ19 страницBells Palsy or Stroke 02.06.2019Emily EresumaОценок пока нет
- Morning Report: Laura Lascurain MD PGY 3 May 1, 2015Документ19 страницMorning Report: Laura Lascurain MD PGY 3 May 1, 2015Emily EresumaОценок пока нет
- TularemiaДокумент19 страницTularemiaEmily EresumaОценок пока нет
- POLYCYTHEMIAДокумент29 страницPOLYCYTHEMIAFaizan KhanОценок пока нет
- Pediatric Hematology LectureДокумент84 страницыPediatric Hematology LectureloitaОценок пока нет
- Sepsis PowerPointДокумент49 страницSepsis PowerPointWonyenghitari GeorgeОценок пока нет
- Pediatrics Osce: Done By: Mohammed I. Alhefzi. Othman M. Omair Dec. 2011Документ71 страницаPediatrics Osce: Done By: Mohammed I. Alhefzi. Othman M. Omair Dec. 2011marina_shawkyОценок пока нет
- Somatization 01.28.2019Документ28 страницSomatization 01.28.2019Emily EresumaОценок пока нет
- Mock Record B-1-2-Well Child VisitsДокумент4 страницыMock Record B-1-2-Well Child VisitsaelteeОценок пока нет
- Lymphadenopathy in Children: Causes, Evaluation and ManagementДокумент34 страницыLymphadenopathy in Children: Causes, Evaluation and ManagementAlchemyAdvisory100% (1)
- Board Prep Metabolics Feb 2019Документ23 страницыBoard Prep Metabolics Feb 2019Emily EresumaОценок пока нет
- History:: Syphilis Is A Disease Caused by The Spirochetal BacteriumДокумент5 страницHistory:: Syphilis Is A Disease Caused by The Spirochetal BacteriumZurkruZОценок пока нет
- EnuresisДокумент31 страницаEnuresisEmily EresumaОценок пока нет
- Morning Report: Jawaria K. Alam, MD/PGY3Документ20 страницMorning Report: Jawaria K. Alam, MD/PGY3Emily EresumaОценок пока нет
- K7 - Supraventricular Tachycardia (SVT)Документ44 страницыK7 - Supraventricular Tachycardia (SVT)Zikri Putra Lan LubisОценок пока нет
- KIDNEY INJURY/Renal Failure: Acute & Chronic: Prof Sampson Antwi Paediatric Nephrologist Sms-Knust/Kath October 2018Документ84 страницыKIDNEY INJURY/Renal Failure: Acute & Chronic: Prof Sampson Antwi Paediatric Nephrologist Sms-Knust/Kath October 2018Effah FestusОценок пока нет
- Metabolic Syndrome GuideДокумент15 страницMetabolic Syndrome GuideMariaEllyNobetaHutabarat100% (1)
- Masalah Gastrointestinal KolestasisДокумент21 страницаMasalah Gastrointestinal KolestasisMuthi'ah Ramadhani AgusОценок пока нет
- Animals Rely On Two Systems For Regulation:: Nervous System Is A System of Nerve Cells Called Neurons. ItДокумент24 страницыAnimals Rely On Two Systems For Regulation:: Nervous System Is A System of Nerve Cells Called Neurons. It陳品汎Оценок пока нет
- 24 HR History 2Документ2 страницы24 HR History 2Arjun KatariaОценок пока нет
- MnemonicsДокумент254 страницыMnemonicsMuhammad Rahim ArshadОценок пока нет
- Cerebral Palsy ExplainedДокумент45 страницCerebral Palsy ExplainedSivakumar Kathuu KarthikeyanОценок пока нет
- Board Prep Emergency Ingestions Dec.2018Документ46 страницBoard Prep Emergency Ingestions Dec.2018Emily EresumaОценок пока нет
- PEDIA 4.1 NephrologyДокумент7 страницPEDIA 4.1 NephrologyAngela CaguitlaОценок пока нет
- Zebras of Neonatal Hypoglycemia 06.09.2014Документ21 страницаZebras of Neonatal Hypoglycemia 06.09.2014Emily EresumaОценок пока нет
- Morning Report: August 28, 2013 Jessica Miller, MD, PGY2Документ30 страницMorning Report: August 28, 2013 Jessica Miller, MD, PGY2Emily EresumaОценок пока нет
- Approach To Viral Hepatitis andДокумент38 страницApproach To Viral Hepatitis andVijay ShankarОценок пока нет
- Pediatrics Vaccine and Milestone ReviewДокумент31 страницаPediatrics Vaccine and Milestone ReviewDrSajid BuzdarОценок пока нет
- Pediatric Shock: A Guide to Identification, Classification and Initial ManagementДокумент20 страницPediatric Shock: A Guide to Identification, Classification and Initial ManagementvgmanjunathОценок пока нет
- Seizures and Epilepsy: Haining Li General Hospital of Ningxia Medical UniversityДокумент50 страницSeizures and Epilepsy: Haining Li General Hospital of Ningxia Medical UniversityArvindhanОценок пока нет
- Nephritic SyndromeДокумент19 страницNephritic SyndromesangheetaОценок пока нет
- Alterations in Neurological, Mental Health and Cognition FunctionsДокумент133 страницыAlterations in Neurological, Mental Health and Cognition Functionsthe4gameОценок пока нет
- Hematological Disorders in Geriatric PatientsДокумент18 страницHematological Disorders in Geriatric PatientsAndre HawkОценок пока нет
- Disorders of Amino Acid MetabolismДокумент11 страницDisorders of Amino Acid MetabolismDiyar AhmadОценок пока нет
- Shelf Prep: Pediatric Patient NotesДокумент9 страницShelf Prep: Pediatric Patient NotesMaría Camila Pareja ZabalaОценок пока нет
- Treating Acute BronchiolitisДокумент3 страницыTreating Acute BronchiolitisHajar Hanis SofiaОценок пока нет
- Pediatric Hematooncology Alarm SymptomsДокумент22 страницыPediatric Hematooncology Alarm SymptomsMuhammad ArifОценок пока нет
- Epilepsy and Seizure DisordersДокумент38 страницEpilepsy and Seizure DisordersMalueth AnguiОценок пока нет
- Approach To Hematuria and Proteinuria in ChildrenДокумент52 страницыApproach To Hematuria and Proteinuria in ChildrenMysheb SS100% (1)
- Pediatric Department Faculty of MedicineДокумент100 страницPediatric Department Faculty of MedicineIrfanОценок пока нет
- Transplantation: Presented by Santhiya K II M.SC Biotechnology 18PBT014Документ54 страницыTransplantation: Presented by Santhiya K II M.SC Biotechnology 18PBT014AbiОценок пока нет
- Erythema Marginatum Chorea: Migratory Polyarthritis Cardiac Involvement Subcutaneous NodulesДокумент27 страницErythema Marginatum Chorea: Migratory Polyarthritis Cardiac Involvement Subcutaneous NodulesMisbah KaleemОценок пока нет
- Immunization ScheduleДокумент2 страницыImmunization SchedulemirojsОценок пока нет
- Lec 2 - Blood VesselsДокумент12 страницLec 2 - Blood VesselsJeffrey LübbertОценок пока нет
- GROUP 3 Case PresentationДокумент35 страницGROUP 3 Case PresentationDinesh KumarОценок пока нет
- Basic Mechanisms Underlying Seizures and EpilepsyДокумент44 страницыBasic Mechanisms Underlying Seizures and EpilepsytaniaОценок пока нет
- Hypocalcemia - Endocrinology AdvisorДокумент14 страницHypocalcemia - Endocrinology AdvisorAliHussainОценок пока нет
- Dermatopathology Quick Reference Guide for Inflammatory Superficial Perivascular DisordersДокумент2 страницыDermatopathology Quick Reference Guide for Inflammatory Superficial Perivascular DisordersBob LoblawОценок пока нет
- PedsCases - Anaphylaxis Emergency TreatmentДокумент5 страницPedsCases - Anaphylaxis Emergency TreatmentSara Ilyas KhanОценок пока нет
- PAT - Remick Spring CE 2014Документ50 страницPAT - Remick Spring CE 2014Nadar RizatullahОценок пока нет
- Syncope: UCI Internal Medicine Core Curriculum - Mini LectureДокумент15 страницSyncope: UCI Internal Medicine Core Curriculum - Mini LecturechandanОценок пока нет
- Pediatric Hypertension Noon Conference 03.20.2019Документ44 страницыPediatric Hypertension Noon Conference 03.20.2019Emily EresumaОценок пока нет
- Board Prep GI Jan 2019Документ32 страницыBoard Prep GI Jan 2019Emily EresumaОценок пока нет
- Morning Report Case Presentation: APRIL 1, 2019Документ14 страницMorning Report Case Presentation: APRIL 1, 2019Emily EresumaОценок пока нет
- Kidney Disorders 03.27.2019Документ33 страницыKidney Disorders 03.27.2019Emily EresumaОценок пока нет
- Pertussis 01.14.2019Документ29 страницPertussis 01.14.2019Emily EresumaОценок пока нет
- Bells Palsy or Stroke 02.06.2019Документ19 страницBells Palsy or Stroke 02.06.2019Emily EresumaОценок пока нет
- Dangers of Vaping 03.15.2019Документ23 страницыDangers of Vaping 03.15.2019Emily EresumaОценок пока нет
- Food Challenge 03.20.2019Документ17 страницFood Challenge 03.20.2019Emily EresumaОценок пока нет
- Board Prep Metabolics Feb 2019Документ23 страницыBoard Prep Metabolics Feb 2019Emily EresumaОценок пока нет
- Case Presentation: Tad MiyaДокумент41 страницаCase Presentation: Tad MiyaEmily EresumaОценок пока нет
- Investing 101 For Residents: RJ Nemeyer MDДокумент12 страницInvesting 101 For Residents: RJ Nemeyer MDEmily EresumaОценок пока нет
- Anemia: Erika Franz-O'Neal PGY-2 Pediatric ResidentДокумент16 страницAnemia: Erika Franz-O'Neal PGY-2 Pediatric ResidentEmily EresumaОценок пока нет
- Ophtho Pearls 03.13.2019Документ17 страницOphtho Pearls 03.13.2019Emily EresumaОценок пока нет
- Tachycardia How To Keep Your Patient Alive in The Middle of The NightДокумент30 страницTachycardia How To Keep Your Patient Alive in The Middle of The NightEmily Eresuma100% (1)
- Somatization 01.28.2019Документ28 страницSomatization 01.28.2019Emily EresumaОценок пока нет
- Board Prep Genetics Dec 2018Документ62 страницыBoard Prep Genetics Dec 2018Emily EresumaОценок пока нет
- Board Prep Emergency Ingestions Dec.2018Документ46 страницBoard Prep Emergency Ingestions Dec.2018Emily EresumaОценок пока нет
- Chronic Granulomatous Disease 01.23.2019Документ10 страницChronic Granulomatous Disease 01.23.2019Emily EresumaОценок пока нет
- Jaundice 11.28.2018Документ13 страницJaundice 11.28.2018Emily EresumaОценок пока нет
- Wilderness Medicine 11.20.2018Документ12 страницWilderness Medicine 11.20.2018Emily EresumaОценок пока нет
- Morning Report: Melanie Nelson, PGY-2Документ25 страницMorning Report: Melanie Nelson, PGY-2Emily EresumaОценок пока нет
- Morning Report: JANUARY 7, 2019 Katie Mailey, Pgy2Документ24 страницыMorning Report: JANUARY 7, 2019 Katie Mailey, Pgy2Emily EresumaОценок пока нет
- Ventilators 11.07.2018Документ38 страницVentilators 11.07.2018Emily EresumaОценок пока нет
- MysteryCase 10.22.18Документ10 страницMysteryCase 10.22.18Emily EresumaОценок пока нет
- Pediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Документ35 страницPediatric Urology Topics Relating To Infants & Toddlers: Danielle Brady, Pgy-2Emily EresumaОценок пока нет
- Morning Report: Lindsey Gakenheimer-Smith MD PGY3Документ20 страницMorning Report: Lindsey Gakenheimer-Smith MD PGY3Emily EresumaОценок пока нет
- Halloween Safety: Dominique ChevalierДокумент21 страницаHalloween Safety: Dominique ChevalierEmily EresumaОценок пока нет
- Morning Report: Wade Harrison, MD, MPHДокумент13 страницMorning Report: Wade Harrison, MD, MPHEmily EresumaОценок пока нет
- Foster Care in Utah: Marlayna DespresДокумент11 страницFoster Care in Utah: Marlayna DespresEmily EresumaОценок пока нет
- Trial Ospe 1 Year: From PPSP UsmkkДокумент43 страницыTrial Ospe 1 Year: From PPSP UsmkkEddy Loo100% (1)
- Obstructive Sleep Apnea Syndromes: Definitions, Epidemiology, Diagnosis, and VariantsДокумент25 страницObstructive Sleep Apnea Syndromes: Definitions, Epidemiology, Diagnosis, and VariantsnatalieОценок пока нет
- Aortic StenosisДокумент14 страницAortic Stenosisjyoti singh100% (3)
- Glomerular Diseases-Part 1Документ68 страницGlomerular Diseases-Part 1hrg79qzwc2Оценок пока нет
- UM XPress Revision in Short Cases PDFДокумент226 страницUM XPress Revision in Short Cases PDFKurouSaki78% (9)
- MUPAS, Grace Geraldine R. - Drug StudyДокумент17 страницMUPAS, Grace Geraldine R. - Drug StudyGrace Geraldine MupasОценок пока нет
- RT Skills ChecklistДокумент3 страницыRT Skills ChecklistMond SantosОценок пока нет
- ACVIM Consensus Guidelines For The Diagnosis and Treatment of Myxomatous Mitral Valve Disease in Dogs.Документ14 страницACVIM Consensus Guidelines For The Diagnosis and Treatment of Myxomatous Mitral Valve Disease in Dogs.Evaldo MamedesОценок пока нет
- Pregnancy Induced Hypertension: Also Called: Toxemia or Pre-Eclampsia or Gestational HypertensionДокумент22 страницыPregnancy Induced Hypertension: Also Called: Toxemia or Pre-Eclampsia or Gestational HypertensionRhuby Pascual AbenojaОценок пока нет
- Ha Sas Lec #6-23 Answer Key PDFДокумент66 страницHa Sas Lec #6-23 Answer Key PDFMaria Jub Mangruban50% (2)
- Xylocaine Dentaland AdrenalineДокумент7 страницXylocaine Dentaland Adrenalinefawwaz FofoОценок пока нет
- 2 - Vascular InjuryДокумент6 страниц2 - Vascular Injuryمحمد عماد عليОценок пока нет
- Happy Family FloaterformДокумент5 страницHappy Family FloaterformWealthMitra Financial ServicesОценок пока нет
- Emerging Therapies in Hfpef 3Документ64 страницыEmerging Therapies in Hfpef 3api-588254706Оценок пока нет
- CtvsДокумент9 страницCtvsManoj KumarОценок пока нет
- Pediatric Cardiovascular System History & ExaminationДокумент74 страницыPediatric Cardiovascular System History & Examinationعبدالله Abdullah IОценок пока нет
- Thyroid FunctionДокумент2 страницыThyroid FunctionVishnuga MohanОценок пока нет
- Contraception: Objective at The End of This Lecture The 5 Year Student Should Be Able ToДокумент22 страницыContraception: Objective at The End of This Lecture The 5 Year Student Should Be Able ToAmmarОценок пока нет
- Informasi Produk Iritero 5 MLДокумент30 страницInformasi Produk Iritero 5 MLWawan MalawatОценок пока нет
- Facility Risk Assessment Form v.2Документ1 страницаFacility Risk Assessment Form v.2Errol Llanes100% (1)
- HEMOSTASISДокумент12 страницHEMOSTASISRyan PedregosaОценок пока нет
- The ESC Textbook of Sports CardiologyДокумент478 страницThe ESC Textbook of Sports CardiologyIBFiS100% (1)
- Altitude Diving PhysiologyДокумент12 страницAltitude Diving PhysiologyKarin Gandeswari100% (1)
- Drugs Used in The Treatment of Congestive Heart FailureДокумент18 страницDrugs Used in The Treatment of Congestive Heart Failurekarina azlia amandaОценок пока нет
- Urine AnalysisДокумент32 страницыUrine AnalysisbnmjgcОценок пока нет
- Normal Chest Radiology Findings and InterpretationДокумент116 страницNormal Chest Radiology Findings and InterpretationSnezana Mihajlovic100% (1)
- Sample COC Nursing Degree-1-1Документ29 страницSample COC Nursing Degree-1-1Ibsa UsmailОценок пока нет
- Sjogren Syndrome: Schirmer TestДокумент2 страницыSjogren Syndrome: Schirmer TestRiena Austine Leonor NarcillaОценок пока нет
- Shelf IM Video SlidesДокумент69 страницShelf IM Video SlidesRuth SanmooganОценок пока нет
- Integrated Therapeutics-Ii For 3 Year STS: Chapter-1Документ69 страницIntegrated Therapeutics-Ii For 3 Year STS: Chapter-1Geleta GalataaОценок пока нет