Академический Документы
Профессиональный Документы
Культура Документы
Ward Round Report 2. MRS.S CVD SH
Загружено:
lie anto0 оценок0% нашли этот документ полезным (0 голосов)
11 просмотров17 страницs
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документs
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
11 просмотров17 страницWard Round Report 2. MRS.S CVD SH
Загружено:
lie antos
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 17
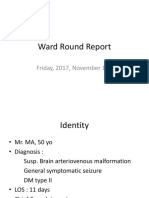
Ward Round Report
Friday, 2017, August 25th
Identity
• Mrs. S, 51 yo
• Diagnosis :
CVD SH (ICH R/ Ganglia basalis Sinistra vol
±27 cc)
HT grade II
• LOS : 8 days
• Chief Complain : unconsciousness
HISTORY TAKING
• Female 51 yo admitted to hospital with chief
complain unconsciousness since 3 days before
admission
• The patient complained suddenly feel headache
• According to her family her left side of the body
more active than the right side since 3 days ago.
• Vomit 1 time consist of food and fluid, blood (-)
• Double vision (-),seizure (-), faver (-), trauma (-)
• Patient had been treated in kotamobagu
hospital
Past History
• History of illness like this before (-)
• Hypertension (+) since 2 years ago when,
doesn’t take medicine regularly.
• Cholesterol, DM, Heart Disease, and kidney
disease were denied.
Physical Examination first day onset
General Examination
– General condition: moderate, Consciousness :
Somnollen
– BP: 190/100 mmHg, MABP : 130 HR: 92 x/m reg, RR:
24x/m , T: 36.6°C
– Conjunctiva : pale (-/-), sclera icteric (-/-)
– JVP ; normal
– Thorax : Rale -/-, Wh -/-, heart sound I/II normal, gallop
-, murmur –
– Abdomen : Flat, normal turgor, peristaltic normal
– Extremities : warm acral
Neurologic Examination
• GCS E3M5V2 (10) Pupil Isocor ø 3 mm/3 mm
Direct light Reflex +/+ Indirect Light Reflex +/+
• Meningeal Sign: nuchal rigidity (-) Laseque
>70/>70 Kerniq >135/>135
• Cranial Nerves: paresis N VII UMN Dextra
impression, N XII UMN Dextra impression
• Motoric State : hemiparesis Dextra impression
MT ↓ N PhyR : +/+/+ ++/++/++ PatR : - -
↓N +/+ ++/++ - -
• Sensoric State :Not evaluated
• Autonomic State : Incontinentia urine et alvi (-)
• GMA : SH
• SSS : (2.5x1)+(2x0)+(2x1)+(0,1x90)-
(3x0)-12 = 1.5 (SH)
Physical Examination 8 th day LOS
General Examination
• General condition: moderate
• Consciousness: compos mentis
• BP: 140/100 mmHg, HR 59 times per minute, RR 18 times per
minute , T 36˚C, SaO2 97%
• Conjunctiva pale (-/-), sclera ikteric (-/-)
• Thorax : Rh -/-, Wh -/-, heart sound I/II normal, gallop -,
murmur -
• Abdomen : Flat, normal turgor, peristaltic normal
• Extremities : warm acral
Neurologic Examination
• GCS E4M6Vafasia
• Pupil round ø 3/3 mm. Direct light Reflex +/+ Indirect Light Reflex
+/+
• Meningeal signs: Nuchal rigidity(-), Lasegue sign >70/>70, Kerniq
sign >135/>135
• Nn. Craniales: paresis N VII UMN dextra, N XII UMN dextra
• Motoric examination:
MS : 1111 5555
1111 5555
MT : ↓ N
↓ N
PhyR : ++/++/++ ++/++/++ PatR : - -
++/++ ++/++ - -
• Sensoric examination: Not evaluated
• Otonom status: urination via catheter
Laboratory Report (18th August 2017)
• Hb : 13.1% • SGOT : 12 U/L
• Ht : 39.5 % • SGPT : 17U/L
• WBC : 10.700 /uL • Ureum : 35 mg/dL
• PLT : 187.000 /uL • Creatinin : 0.8 mg/dL
• RBC : 5.690.000 /uL • GDS : 99 mg/dL
• Na : 138 mEq/L
• K : 3.7 mEq/L
• Cl : 105.0 mEq/L
Laboratory Report (22th August 2017)
• Fasting Blood sugar : 129 mg/dL
• Uric acid : 5.6 mg/dL
• Cholesterol : 186 mg/dL
• HDL : 33 mg/dL
• LDL : 135 mg/dL
• Trigliseride : 92 mg/dL
• Albumin : 3.74 g/dL
Chest X-Ray
Brain CT
Brain CT
EKG
• Normal sinus rhytm
Diagnosis
• unconsciousness ec CVD SI (ICH Ganglia
basalis vol 27 cc ) 10th day onset
• Hypertension grade II
Treatment
• Family education
• Bed rest + head elevation 30˚
• Mobilization right and left side every 2 hours
• Chest physiotherapy + OH
• IVFD NaCl 0.9% 500cc 20 gtt/mnts
• Simvastatin 20mg 0-0-1
• Amlodipine 10mg 1-0-0
• Valsartan 80mg 0-0-1
• Inj ranitidine 2x50mg IV
• PCT 3x500mg P.O.
• Lactulac syr 0-0-CII
Вам также может понравиться
- Depression in Parkinson's Disease Ppt1Документ14 страницDepression in Parkinson's Disease Ppt1lie antoОценок пока нет
- Status Epileptikus Morning ReportДокумент16 страницStatus Epileptikus Morning Reportlie antoОценок пока нет
- IVH + Edema CerebriДокумент16 страницIVH + Edema Cerebrilie antoОценок пока нет
- Upload 1cДокумент11 страницUpload 1clie antoОценок пока нет
- Ward ReportДокумент13 страницWard Reportlie antoОценок пока нет
- NIH Public Access: Author ManuscriptДокумент12 страницNIH Public Access: Author Manuscriptlie antoОценок пока нет
- Upload 1aДокумент12 страницUpload 1alie antoОценок пока нет
- Upload 3Документ12 страницUpload 3lie antoОценок пока нет
- Ward Round ReportДокумент13 страницWard Round Reportlie antoОценок пока нет
- Mrs. MW/ 82 Yo/ DX: Cerebral Haemorrhage Onset 1 Day, Hypertension EmergencyДокумент17 страницMrs. MW/ 82 Yo/ DX: Cerebral Haemorrhage Onset 1 Day, Hypertension Emergencylie antoОценок пока нет
- Delayed Recompression For Decompression Sickness: Retrospective AnalysisДокумент13 страницDelayed Recompression For Decompression Sickness: Retrospective Analysislie antoОценок пока нет
- Pone 0050079 PDFДокумент6 страницPone 0050079 PDFlie antoОценок пока нет
- Primary Survey: A: Clear B: RR 24x/m Adecuate, Simetris D/S C: HR 88x/m Reguler, Adecuate D: Verbal Respons E: HeadДокумент17 страницPrimary Survey: A: Clear B: RR 24x/m Adecuate, Simetris D/S C: HR 88x/m Reguler, Adecuate D: Verbal Respons E: Headlie antoОценок пока нет
- Ward Round Report10 Nov AVMДокумент21 страницаWard Round Report10 Nov AVMlie antoОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Health Assessment SAS Session 14Документ9 страницHealth Assessment SAS Session 14Maria Jub MangrubanОценок пока нет
- Antihypertensive Drugs - Classification & MechanismДокумент1 страницаAntihypertensive Drugs - Classification & MechanismAhmed YT100% (1)
- Biology For The IB Diploma - Option D - Human PhysiologyДокумент57 страницBiology For The IB Diploma - Option D - Human PhysiologyjjkjljОценок пока нет
- Five"EFFICACY OF GANDHARVAHASTADI KASHAYAM IN THE MANAGEMENT OF ESSENTIAL HYPERTENSION (UCCHA - RAKTHACHAAPA)Документ12 страницFive"EFFICACY OF GANDHARVAHASTADI KASHAYAM IN THE MANAGEMENT OF ESSENTIAL HYPERTENSION (UCCHA - RAKTHACHAAPA)Pradeep SambandamОценок пока нет
- The DASH Diet and Blood PressureДокумент8 страницThe DASH Diet and Blood PressureJosefina OrtegaОценок пока нет
- CSOMДокумент32 страницыCSOMDarwin LlanesОценок пока нет
- Sample CCS-P Exam - (Multiple-Choice Questions)Документ5 страницSample CCS-P Exam - (Multiple-Choice Questions)shyamsunder_nagula100% (1)
- Reading Comprehension ITP 1Документ38 страницReading Comprehension ITP 1Reini KurniawatiОценок пока нет
- Case Report: Severe Vitamin B12 Deficiency in Pregnancy Mimicking HELLP SyndromeДокумент5 страницCase Report: Severe Vitamin B12 Deficiency in Pregnancy Mimicking HELLP SyndromeSuci Triana PutriОценок пока нет
- Case Study in PPHДокумент16 страницCase Study in PPHMar Ordanza0% (1)
- Zhan ZhuangДокумент13 страницZhan ZhuangBrian ColborneОценок пока нет
- The Heartmath Approach To Managing Hypertension - Bruce WilsonДокумент113 страницThe Heartmath Approach To Managing Hypertension - Bruce WilsonDaniel Ianas100% (1)
- Climate ChangeДокумент2 страницыClimate ChangeJeymar BenignoОценок пока нет
- Serum Uric Acid and Chronic Kidney Disease The Role of HypertensionДокумент8 страницSerum Uric Acid and Chronic Kidney Disease The Role of HypertensionAdam Adachi SanОценок пока нет
- Exit Exam WolaytaДокумент18 страницExit Exam WolaytaMilkii Du Nikus100% (1)
- Case Analysis: Pre-OperativeДокумент12 страницCase Analysis: Pre-OperativeMaria ThereseОценок пока нет
- Diet During Adulthood UbДокумент34 страницыDiet During Adulthood UbBeatrice Chen0% (1)
- PHD Thesis On Coronary Artery DiseaseДокумент5 страницPHD Thesis On Coronary Artery Diseasebdg9hkj6100% (1)
- Cronic Heart Failure - EscДокумент55 страницCronic Heart Failure - EscRisti Graharti100% (1)
- A Case Presentation of Diabetes Mellitus Type 2 Uncontrolled Non-Healing WoundДокумент67 страницA Case Presentation of Diabetes Mellitus Type 2 Uncontrolled Non-Healing Woundashamy acolОценок пока нет
- Cmca Lec Prelim ReviewerДокумент26 страницCmca Lec Prelim ReviewerCrystal MiranaОценок пока нет
- Buddiga, 2014 Cardiovascular System Anatomy - Overview, Gross Anatomy, Natural VariantsДокумент13 страницBuddiga, 2014 Cardiovascular System Anatomy - Overview, Gross Anatomy, Natural VariantsAzilu FalaОценок пока нет
- Literature Review: Terapi Relaksasi Otot Progresif Terhadap Penurunan Tekanan Darah Pada Pasien HipertensiДокумент8 страницLiterature Review: Terapi Relaksasi Otot Progresif Terhadap Penurunan Tekanan Darah Pada Pasien Hipertensinadia hanifaОценок пока нет
- ACT 4 Scene 1 - HypertensionДокумент32 страницыACT 4 Scene 1 - Hypertensionsameersidana18Оценок пока нет
- GSIS v. CalumpianoДокумент2 страницыGSIS v. CalumpianoKei Sha100% (1)
- Science Reporting: Henrylito D. TacioДокумент12 страницScience Reporting: Henrylito D. TacioJay Mark SausaОценок пока нет
- CME Quiz 2019 Nov Issue 9Документ3 страницыCME Quiz 2019 Nov Issue 9Basil al-hashaikehОценок пока нет
- Clonidine DosisДокумент2 страницыClonidine Dosispetersouisa6454Оценок пока нет
- A Case Study On Hypertensive Urgency - Group 2 Section 3BДокумент48 страницA Case Study On Hypertensive Urgency - Group 2 Section 3BhernandezmarianneroseОценок пока нет
- Kidney Maybe Super No WWWДокумент205 страницKidney Maybe Super No WWWZsheib Bub100% (1)