Академический Документы
Профессиональный Документы
Культура Документы
Age-Related Macular Disease: Fitriani Umi Hasanah 201820401011121 Pembimbing: Dr. Fatin Hamamah, SP.M
Загружено:
Kim Nayoung0 оценок0% нашли этот документ полезным (0 голосов)
82 просмотров28 страницARMD
Оригинальное название
ARMD
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документARMD
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
82 просмотров28 страницAge-Related Macular Disease: Fitriani Umi Hasanah 201820401011121 Pembimbing: Dr. Fatin Hamamah, SP.M
Загружено:
Kim NayoungARMD
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 28
Age-Related Macular Disease
Fitriani Umi Hasanah
201820401011121
Pembimbing:
dr. Fatin Hamamah, Sp.M
Definition
• ARMD is a degenerative disease of the central part of the retina—
known as the macula—that results in a loss of central vision, which is
essential for most daily activities
• It is characterized by a loss of visual acuity caused by degeneration of
the choriocapillaris, retinal pigment epithelium (RPE), and
photoreceptors, usually beginning with drusen and pigmentary
changes in Bruch's membrane
Prevalency
• The condition, which affects 30 million to 50 million people
worldwide, is the leading cause of irreversible blindness in developed
countries in people aged 50 years and older
• The prevalence of ARMD increases exponentially every decade after
age 50
Etiology
• genetic,
• environmental,
• metabolic, and
• functional factors; including aging, family history, smoking, high blood
pressure, obesity, hypercholesterolemia, and arteriosclerosis, sun
exposure, atherosclerosis, hypertension, diabetes, polypharmacy,
alcohol, ethnicity, hypothyroidism, and C-reactive protein
Patophysiology
Stages of ARMD
• Early stages of ARMD are characterized by a macula that has
yellowish subretinal deposits (drusen) and/or increased pigment
• Patients with early ARMD have stable visual acuity for many years,
and loss of vision is gradual
American Academy of Ophtalmology
Retina/Vitreous Panel. Preferred Practice
AREDS Classification of ARMD Pattern Guidelines. Age-Related Macular
Degeneration. San Fransisco, CA: American
Academy of Ophtalmology; 2014
Category Designation Description
No ARMDNo or few small drusen
1
(<63 μm in diameter)
Multiple small drusen (<20), a few
2 Early intermediate drusen (63–124 μm in
diameter), or RPE abnormalities
Extensive intermediate drusen, ≥1
large drusen (125 μm in diameter),
3 Intermediate
or geographic atrophy not involving
center of fovea
Geographic atrophy or neovascular
4 Advanced
maculopathy
AREDS: Age-Related Eye Disease Study; ARMD: age-related macular degeneration; RPE: retinal pigment
epithelium.
• Early AMD. Early AMD is diagnosed by the presence of medium-sized drusen, which are
about the width of an average human hair. People with early AMD typically do not have
vision loss.
• Intermediate AMD. People with intermediate AMD typically have large drusen, pigment
changes in the retina, or both. Again, these changes can only be detected during an eye
exam. Intermediate AMD may cause some vision loss, but most people will not
experience any symptoms.
• Late AMD. In addition to drusen, people with late AMD have vision loss from damage to
the macula. There are two types of late AMD:
• In geographic atrophy (also called dry AMD), there is a gradual breakdown of the light-sensitive
cells in the macula that convey visual information to the brain, and of the supporting tissue
beneath the macula. These changes cause vision loss.
• In neovascular AMD (also called wet AMD), abnormal blood vessels grow underneath the retina.
(“Neovascular” literally means “new vessels.”) These vessels can leak fluid and blood, which may
lead to swelling and damage of the macula. The damage may be rapid and severe, unlike the more
gradual course of geographic atrophy. It is possible to have both geographic atrophy and
neovascular AMD in the same eye, and either condition can appear first.
1. DRY ARMD
• is also known as nonexudative, nonneovascular, or atrophic ARMD
• more common form of ARMD, seen in about 90% of cases
• Vision loss in dry ARMD is gradual and usually is associated with
moderate visual impairment, as well as functional limitations
including fluctuating vision, difficulty reading, and limited vision at
night or under conditions of reduced illumination
• Upon examination, the macula shows areas of depigmentation
• Early to intermediate nonexudative AMD: Significant for the presence
of multiple drusen for early AMD. For intermediate AMD, drusen may
appear confluent with significant pigment changes and pigment
accumulation in the posterior pole. In addition, the retinal pigment
epithelium (RPE) often appears atrophic, with easier visualization of
the underlying choroid vascular plexus
• Difficulty with night vision and with changing light conditions
(specifically, changes in Amsler grid self-evaluation and trouble with
reading)
• Visual fluctuation (ie, some days, vision is poor; other days, vision
appears improved)
• Difficulty with reading and making out faces
• Metamorphopsia (distortion of visual images): Not a major patient
complaint for dry AMD, but it may be present as the atrophy slowly
progresses.
Management dry AMD
• Antioxidant vitamin and mineral supplements (vitamin A, vitamin E,
zinc, and lutein)
• Screening for impaired visual acuity
• Wraparound shades (eg, orange-tinted, blue blocker lenses): Effective
solution for delayed dark adaptation and to protect eyes from direct
sunlight
• Avoidance/cessation of tobacco use
• Frequent follow-up for risk assessment of conversion to exudative
AMD
2. WET ARMD
• also referred to as exudative or neovascular ARMD, accounts for
about 10% of cases
• its presence usually indicates a more advanced disease state, and it is
associated with rapid distortion and a sudden loss of central vision
over a period of weeks to months
• he eyes have two times the expected prevalence of vitreomacular
adhesion and are less likely to have a posterior vitreous detachment.
• Fluid and exudate may accumulate underneath the retina in patients
with neovascular ARMD, resulting in severe macular edema
Diagnosis WET AMD
After a thorough dilated examination of the fundus with slit lamp
biomicroscopy, the following imaging studies are frequently performed
on many patients with signs and symptoms of exudative AMD:
• Color photography of the fundus
• Fluorescein angiography (FA) - Helps to identify and confirm the
source of CNV
• Optical coherence tomography (OCT) - Can identify soft drusen, RPE
detachments, subretinal and intraretinal fluid, CNV, and cystoid
macular edema; can accurately measure foveal and macular
thickness; and can demonstrate the integrity of the photoreceptor
and RPE layers
Management WET AMD
1. Antiangiogenic agents
Animal and clinical studies have established vascular endothelial growth
factor (VEGF) as a key mediator in ocular angiogenesis.Therefore, particular
attention has been focused on the development of pharmaceutical agents to
block or neutralize VEGF expression. The following agents, delivered via
intravitreal injection, have been proven effective in clinical trials:
• Pegaptanib sodium
• Ranibizumab
• Bevacizumab
• Aflibercept
2. Laser treatments
• Laser treatments include the following:
• Thermal laser photocoagulation - Until the advent of anti-VEGF
agents, ophthalmologists traditionally used thermal laser destruction
of CNV as the primary treatment of exudative AMD.
• Photodynamic therapy with verteporfin (PDT) - To avoid creating a
central, blinding scotoma when treating subfoveal CNV with thermal
lasers, clinicians turned to PDT; effective in some forms of CNV,
although its use is sometimes limited by cost.
• If left untreated, the neovascular membrane forms a big scar in the
macular area, resulting in a sudden decrease in central vision
• Choroidal neovascularization (CNV) is an advanced stage of wet
ARMD that can lead to the development of polypoidal choroidal
vasculopathy
• he condition progresses from drusen to the development of CNV,
whereby the choriocapillaries cross Bruch's membrane and spread
laterally within the planes of these lesions
Drusen
• Drusen are focal deposits of extracellular debris that typically form
between the basal lamina of the RPE and the inner collagenous layer
of Bruch's membrane
• generally round and yellowish in color
• These lesions, which are considered the hallmark of ARMD and are
characteristic of the aging eye and age-related maculopathy, can be
detected through various assays
• Drusen are classified as hard or soft, depending upon their borders
and the level of risk they confer on progression of ARMD
• Soft drusen are more commonly found in the macula and pose a
higher risk of ARMD development
• They are slightly larger than hard drusen and do not have well-
defined margins
• Hard drusen tend to be smaller and well defined. The distinct features
of the druse may give an indication of the stage of ARMD
• Drusen are known to contain lipids, carbohydrates, zinc, and at least
129 different proteins, including extracellular matrix
• The molecules trapped in drusen have varying roles, including the
processing of extracellular enzymes, the stigmata of formative
processes (e.g., extrusion or secretion of cellular materials), and
cellular invasion
• Charles Bonnet syndrome is a common side effect of vision loss in
people with AMD. However, it often goes away a year to 18 months
after it begins. In the meantime, there are things you can do to
reduce hallucinations. Many people find the hallucinations occur
more frequently in evening or dim light. Turning on a light or
television may help. It may also help to blink, close your eyes, or focus
on a real object for a few moments
Prognosis
• Prognosis dari degenerasi makula dengan tipe eksudat lebih buruk di
banding dengan degenerasi makula tipe non eksudat. Prognosis dapat
didasarkan pada terapi, tetapi belum ada terapi yang bernilai efektif
sehingga kemungkinan untuk sembuh total sangat kecil
Вам также может понравиться
- The Skeffington Perspective of the Behavioral Model of Optometric Data Analysis and Vision CareОт EverandThe Skeffington Perspective of the Behavioral Model of Optometric Data Analysis and Vision CareОценок пока нет
- Soal OFKOMДокумент3 страницыSoal OFKOMDian ArianiОценок пока нет
- Limbal DermoidДокумент4 страницыLimbal DermoidPranjali ChhayaОценок пока нет
- Hey, Doc! What’S Wrong with My Eye?: A General Guide to Eye SymptomsОт EverandHey, Doc! What’S Wrong with My Eye?: A General Guide to Eye SymptomsОценок пока нет
- 14th SOM LAMPUNG 2020 PROPOSALДокумент23 страницы14th SOM LAMPUNG 2020 PROPOSALnovitaОценок пока нет
- Direct and Indirect FinalДокумент31 страницаDirect and Indirect Finalmeenali karnОценок пока нет
- Aao Bab 4Документ3 страницыAao Bab 4ria mutiaraОценок пока нет
- Soal Subdivisi Roo Eyelid NeoplasmДокумент8 страницSoal Subdivisi Roo Eyelid NeoplasmBudhi KaromaОценок пока нет
- Anterior Chamber Angle Assessment TechniquesДокумент29 страницAnterior Chamber Angle Assessment TechniquesSabyasachi100% (4)
- 1 - Perbandingan Teknik Endoscopic Third VentriculostomyДокумент10 страниц1 - Perbandingan Teknik Endoscopic Third VentriculostomyKathryn TurnerОценок пока нет
- Database Member CIMSA UNISSULA Update 2 Agustus 2014Документ51 страницаDatabase Member CIMSA UNISSULA Update 2 Agustus 2014persijapqОценок пока нет
- Catarata. Kanski.Документ33 страницыCatarata. Kanski.leidoskyОценок пока нет
- Anophthalmia and MicrophthalmiaДокумент8 страницAnophthalmia and MicrophthalmiaLjubomirErdoglijaОценок пока нет
- Daftar Ebook THTДокумент3 страницыDaftar Ebook THTPrathita AmandaОценок пока нет
- Diabetic Retinopathy - Classification and Clinical Features - UpToDateДокумент38 страницDiabetic Retinopathy - Classification and Clinical Features - UpToDateRachmatBimanjayaОценок пока нет
- Choice of Surgical Therapy For Perforating Corneal UlcerДокумент23 страницыChoice of Surgical Therapy For Perforating Corneal Ulcerhavriza vitresia100% (1)
- MataДокумент163 страницыMataadelОценок пока нет
- Penetrating Keratoplasty StepsДокумент57 страницPenetrating Keratoplasty StepsVishwajeetОценок пока нет
- Aao Asli FixДокумент78 страницAao Asli FixAndy William100% (1)
- International Council of Ophthalmology's Ophthalmology Surgical Competency Assessment Rubric (ICO-OSCAR)Документ7 страницInternational Council of Ophthalmology's Ophthalmology Surgical Competency Assessment Rubric (ICO-OSCAR)Jose Antonio Fuentes VegaОценок пока нет
- Correlation of Retinal Structural Alteration With Retinal Sensitivity Loss: A Prospective StudyДокумент26 страницCorrelation of Retinal Structural Alteration With Retinal Sensitivity Loss: A Prospective StudyAbhishek KothariОценок пока нет
- Corne A: Dr. Yulia Fitriani, SPMДокумент47 страницCorne A: Dr. Yulia Fitriani, SPMEdsel QasswaraОценок пока нет
- RetinaДокумент82 страницыRetinafebienaОценок пока нет
- Soal Infeksi Immunology 2019Документ7 страницSoal Infeksi Immunology 2019Reinhard TuerahОценок пока нет
- Second Announcement INAVRS Meeting 2023 INANOS IOASДокумент2 страницыSecond Announcement INAVRS Meeting 2023 INANOS IOASAndi Ayu LestariОценок пока нет
- Soal AAO PO Chapter 18Документ3 страницыSoal AAO PO Chapter 18Defayudina Dafilianty RosatariaОценок пока нет
- Cataract Classification 2003Документ8 страницCataract Classification 2003Abdelrahman M. AlnweiriОценок пока нет
- Presentasi Low VisionДокумент30 страницPresentasi Low VisionAySa AysaОценок пока нет
- Retina Examination and Drawing: CEH Retinal TeamДокумент39 страницRetina Examination and Drawing: CEH Retinal TeamrzmОценок пока нет
- CATARACTДокумент25 страницCATARACTDea NabilaОценок пока нет
- UntitledДокумент24 страницыUntitledLeo LukitoОценок пока нет
- Cataract 20surgery 2029 05 2008 131224024457 Phpapp01Документ61 страницаCataract 20surgery 2029 05 2008 131224024457 Phpapp01Bboy ToonОценок пока нет
- Instrumen SICS (Small Incision Cataract Surgery)Документ2 страницыInstrumen SICS (Small Incision Cataract Surgery)roifdyahОценок пока нет
- 94 - CH 10 - Symptoms in Heterophoria and Heterotropia and The Psychological Effects of Strabismus P. 153-157Документ5 страниц94 - CH 10 - Symptoms in Heterophoria and Heterotropia and The Psychological Effects of Strabismus P. 153-157Catleya ProtacioОценок пока нет
- Operasi Monokular Recess Resect Dengan Teknik: Hangback Pada Exotropia Deviasi BesarДокумент10 страницOperasi Monokular Recess Resect Dengan Teknik: Hangback Pada Exotropia Deviasi BesarBlack Clover IdОценок пока нет
- Glaucoma GuidelinesДокумент28 страницGlaucoma GuidelinesRina RostianaОценок пока нет
- RAPDДокумент2 страницыRAPDAlpascaFirdausОценок пока нет
- Trauma Dan Kegawatdaruratan MataДокумент92 страницыTrauma Dan Kegawatdaruratan MataM Isyhaduul IslamОценок пока нет
- Observations During Fundus ExaminationДокумент3 страницыObservations During Fundus ExaminationAn'umillah Arini ZidnaОценок пока нет
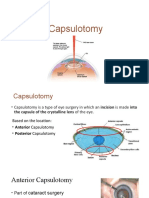
- CapsulotomyДокумент15 страницCapsulotomyAdrian PearlОценок пока нет
- Subluksasi LensaДокумент12 страницSubluksasi LensaDede GunawanОценок пока нет
- Orbital Fractures 1387 2008Документ63 страницыOrbital Fractures 1387 2008AyuAnatrieraОценок пока нет
- Presentasi Kasus Glaukoma AkutДокумент24 страницыPresentasi Kasus Glaukoma AkutHendrawan Ariwibowo100% (1)
- Telaah Kritis Jurnal Oftalmologi - Povidone Iodine + DeksamethasoneДокумент4 страницыTelaah Kritis Jurnal Oftalmologi - Povidone Iodine + DeksamethasoneKurnia22Оценок пока нет
- Leukocoria 2016Документ35 страницLeukocoria 2016DiskaAstarini100% (1)
- Journal Reading - Avizena Muhammad Zamzam - CPPDS Mata UnsriДокумент27 страницJournal Reading - Avizena Muhammad Zamzam - CPPDS Mata UnsriwidyawirapОценок пока нет
- Refractive Errors & Refractive SurgeryДокумент97 страницRefractive Errors & Refractive SurgeryDr-Fadi AlkayyaliОценок пока нет
- Managing Complications in Glaucoma SurgeryДокумент121 страницаManaging Complications in Glaucoma Surgeryshetya_8212Оценок пока нет
- Referat Romzan Retinopathy of PrematurityДокумент46 страницReferat Romzan Retinopathy of Prematurityromzanr97Оценок пока нет
- Board Januari 2009 Unair: GlaukomaДокумент6 страницBoard Januari 2009 Unair: GlaukomaRizky AgustriaОценок пока нет
- Ophtha PCT Foundation BatchДокумент5 страницOphtha PCT Foundation BatchAnas ChaudharyОценок пока нет
- Diagram For Ophtal NoteДокумент7 страницDiagram For Ophtal NoteSiam Weng LoongОценок пока нет
- Tape Stripping by VyasДокумент22 страницыTape Stripping by VyasvunnamnareshОценок пока нет
- Pemeriksaan GonioskopiДокумент26 страницPemeriksaan GonioskopiMuhammad Mu'amar HabibieОценок пока нет
- AmblyopiaДокумент33 страницыAmblyopiaSujon PaulОценок пока нет
- Corneal Drawing and Other StructureДокумент2 страницыCorneal Drawing and Other StructureOden Mahyudin50% (2)
- Correlation Between Body Mass Index and Intraocular Pressure at Eye Clinic Mangusada Hospital, BaliДокумент3 страницыCorrelation Between Body Mass Index and Intraocular Pressure at Eye Clinic Mangusada Hospital, BaliKarina NathaniaОценок пока нет
- Clinical Trial Design Kuliah MKDU 2020Документ51 страницаClinical Trial Design Kuliah MKDU 2020Christine100% (1)
- Biokimia Dan Fisiologi LensaДокумент33 страницыBiokimia Dan Fisiologi LensaNurul FebrianiОценок пока нет
- Targeted Therapy in Age-Related Macular Degeneration (AMD)Документ7 страницTargeted Therapy in Age-Related Macular Degeneration (AMD)adibashafique_214280Оценок пока нет
- Eye Screening Support SystemДокумент70 страницEye Screening Support Systembereketab demmelashОценок пока нет
- Ebook Atlas of Retinal Oct Optical Coherence Tomography PDF Full Chapter PDFДокумент67 страницEbook Atlas of Retinal Oct Optical Coherence Tomography PDF Full Chapter PDFcharles.schmidt276100% (26)
- Kanski'S: Clinical OphthalmologyДокумент504 страницыKanski'S: Clinical OphthalmologyMohin hossain100% (1)
- Jurnal Vitamin CДокумент15 страницJurnal Vitamin CbethjohОценок пока нет
- Faktor Resiko AmdДокумент31 страницаFaktor Resiko AmdKarina BudijantoОценок пока нет
- Homeo Eye DiseaseДокумент15 страницHomeo Eye DiseaseAlbena Trifonova100% (3)
- InTech - ElectroretinogramsДокумент250 страницInTech - ElectroretinogramsriveliОценок пока нет
- CELMA-ELC LED WG (SM) 011 ELC CELMA Position Paper Optical Safety LED Lighting Final 1st Edition July2011 PDFДокумент18 страницCELMA-ELC LED WG (SM) 011 ELC CELMA Position Paper Optical Safety LED Lighting Final 1st Edition July2011 PDFFadi Mohd ShaherОценок пока нет
- Chapter 6.8 Yanoff & DukerДокумент7 страницChapter 6.8 Yanoff & Dukerimran_india12Оценок пока нет
- ICO International Clinical Guidelines: List of Guidelines AvailableДокумент74 страницыICO International Clinical Guidelines: List of Guidelines AvailableOvidiu Rusu100% (1)
- Age Related Macular DegenerationДокумент26 страницAge Related Macular DegenerationRebecca WongОценок пока нет
- Afmg Ophtha Images - 2021Документ189 страницAfmg Ophtha Images - 2021Yesha PatelОценок пока нет
- Eye and Vision DisordersДокумент19 страницEye and Vision DisordersTeena Duray100% (3)
- Atlas de Enfermedades Maculares de GASSДокумент1 357 страницAtlas de Enfermedades Maculares de GASSNidia M. Quispe RodríguezОценок пока нет
- Ebook Ocular Pathology PDF Full Chapter PDFДокумент67 страницEbook Ocular Pathology PDF Full Chapter PDFshannon.boersma620100% (25)
- Nanotechnology-Based Ocular Drug Delivery Systems: Recent Advances and Future ProspectsДокумент39 страницNanotechnology-Based Ocular Drug Delivery Systems: Recent Advances and Future ProspectsLateepheart YakubОценок пока нет
- Heal Your Eye Problems With Herbs, Minerals and VitaminsДокумент117 страницHeal Your Eye Problems With Herbs, Minerals and VitaminsAadilОценок пока нет
- Bionic Eye ReportДокумент18 страницBionic Eye Reportgagandeep_saluja_2Оценок пока нет
- Myopia APDF PDFДокумент14 страницMyopia APDF PDFRao Sab100% (1)
- Director or Vice PresidentДокумент10 страницDirector or Vice Presidentapi-121302781Оценок пока нет
- I Notes RETINA PDFДокумент251 страницаI Notes RETINA PDFFelipe renquenОценок пока нет
- Europian Medicin Agency For EyleaДокумент83 страницыEuropian Medicin Agency For EyleabangunОценок пока нет
- EURETINA - Paris19 Final Programme PDFДокумент176 страницEURETINA - Paris19 Final Programme PDFPamela MukhopadhyayОценок пока нет
- LuteinДокумент42 страницыLuteinNgô HằngОценок пока нет
- Stargardt DiseaseДокумент9 страницStargardt DiseaseEstefhany SCОценок пока нет
- By Prapatsorn Patikulsila, MD.: Ophthalmology AbbreviationsДокумент4 страницыBy Prapatsorn Patikulsila, MD.: Ophthalmology AbbreviationsDoaa SaifОценок пока нет
- 12 Kasper Notes 2020 OphthalmologyДокумент33 страницы12 Kasper Notes 2020 OphthalmologyMohamed Rikarz Ahamed RikarzОценок пока нет
- Vol 2 Retinal AtlasДокумент252 страницыVol 2 Retinal AtlasDra. Mitzy Torres - RetinólogaОценок пока нет
- Advances in The Treatment of Age-Related Macular Degeneration (AMD)Документ22 страницыAdvances in The Treatment of Age-Related Macular Degeneration (AMD)Ega Gumilang SugiartoОценок пока нет