Академический Документы
Профессиональный Документы
Культура Документы
Hyperlipidemia
Загружено:
maritza0 оценок0% нашли этот документ полезным (0 голосов)
274 просмотров22 страницыThe document discusses lipids and lipoproteins such as LDL, HDL, and triglycerides; causes and dietary sources of hyperlipidemia; hereditary causes such as familial hypercholesterolemia; goals and treatment for hyperlipidemia including lifestyle changes and medications; and presents three case studies to demonstrate how lipid goals and treatment would be determined based on a patient's risk factors.
Исходное описание:
Chylomicrons transport fats from the intestinal mucosa to the liver
In the liver, the chylomicrons release triglycerides and some cholesterol and become low-density lipoproteins (LDL).
LDL then carries fat and cholesterol to the body’s cells.
High-density lipoproteins (HDL) carry fat and cholesterol back to the liver for excretion.
Авторское право
© © All Rights Reserved
Доступные форматы
PPT, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документThe document discusses lipids and lipoproteins such as LDL, HDL, and triglycerides; causes and dietary sources of hyperlipidemia; hereditary causes such as familial hypercholesterolemia; goals and treatment for hyperlipidemia including lifestyle changes and medications; and presents three case studies to demonstrate how lipid goals and treatment would be determined based on a patient's risk factors.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
274 просмотров22 страницыHyperlipidemia
Загружено:
maritzaThe document discusses lipids and lipoproteins such as LDL, HDL, and triglycerides; causes and dietary sources of hyperlipidemia; hereditary causes such as familial hypercholesterolemia; goals and treatment for hyperlipidemia including lifestyle changes and medications; and presents three case studies to demonstrate how lipid goals and treatment would be determined based on a patient's risk factors.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPT, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 22
Hyperlipidemia
Michele Ritter, M.D.
Argy Resident – February, 2007
The story of lipids
Chylomicrons transport fats from the intestinal
mucosa to the liver
In the liver, the chylomicrons release triglycerides
and some cholesterol and become low-density
lipoproteins (LDL).
LDL then carries fat and cholesterol to the body’s
cells.
High-density lipoproteins (HDL) carry fat and
cholesterol back to the liver for excretion.
The story of lipids (cont.)
When oxidized LDL cholesterol gets high,
atheroma formation in the walls of arteries
occurs, which causes atherosclerosis.
HDL cholesterol is able to go and remove
cholesterol from the atheroma.
Atherogenic cholesterol → LDL, VLDL, IDL
Atherosclerosis
Causes of Hyperlipidemia
Diet Obstructive liver
Hypothyroidism disease
Nephrotic syndrome Acute heaptitis
Anorexia nervosa Systemic lupus
Obstructive liver erythematousus
disease AIDS (protease
Obesity inhibitors)
Diabetes mellitus
Pregnancy
Dietary sources of Cholesterol
Type of Fat Main Source Effect on
Cholesterol levels
Monounsaturated Olives, olive oil, canola oil, peanut oil, Lowers LDL, Raises
cashews, almonds, peanuts and most HDL
other nuts; avocados
Polyunsaturated Corn, soybean, safflower and cottonseed Lowers LDL, Raises
oil; fish HDL
Saturated Whole milk, butter, cheese, and ice cream; Raises both LDL and
red meat; chocolate; coconuts, coconut HDL
milk, coconut oil , egg yolks, chicken skin
Trans Most margarines; vegetable shortening; Raises LDL
partially hydrogenated vegetable oil; deep-
fried chips; many fast foods; most
commercial baked goods
Hereditary Causes of Hyperlipidemia
Familial Hypercholesterolemia
Codominant genetic disorder, coccurs in heterozygous form
Occurs in 1 in 500 individuals
Mutation in LDL receptor, resulting in elevated levels of LDL at birth and
throughout life
High risk for atherosclerosis, tendon xanthomas (75% of patients), tuberous
xanthomas and xanthelasmas of eyes.
Familial Combined Hyperlipidemia
Autosomal dominant
Increased secretions of VLDLs
Dysbetalipoproteinemia
Affects 1 in 10,000
Results in apo E2, a binding-defective form of apoE (which usually plays
important role in catabolism of chylomicron and VLDL)
Increased risk for atherosclerosis, peripheral vascular disease
Tuberous xanthomas, striae palmaris
Checking lipids
Nonfasting lipid panel
measures HDL and total cholesterol
Fasting lipid panel
Measures HDL, total cholesterol and triglycerides
LDL cholesterol is calculated:
LDL cholesterol = total cholesterol – (HDL + triglycerides/5)
When to check lipid panel
Two different Recommendations
Adult Treatment Panel (ATP III) of the National Cholesterol
Education Program (NCEP)
Beginning at age 20: obtain a fasting (9 to 12 hour) serum lipid profile
consisting of total cholesterol, LDL, HDL and triglycerides
Repeat testing every 5 years for acceptable values
United States Preventative Services Task Force
Women aged 45 years and older, and men ages 35 years and older
undergo screening with a total and HDL cholesterol every 5 years.
If total cholesterol > 200 or HDL <40, then a fasting panel should be
obtained
Cholesterol screening should begin at 20 years in patients with a
history of multiple cardiovascular risk factors, diabetes, or family
history of either elevated cholesteral levels or premature
cardiovascular disease.
Goals for Lipids
LDL HDL
< 100 →Optimal < 40 → Low
100-129 → Near optimal ≥ 60 → High
130-159 → Borderline Serum Triglycerides
160-189→ High < 150 → normal
≥ 190 → Very High 150-199 → Borderline
Total Cholesterol 200-499 → High
< 200 → Desirable ≥ 500 → Very High
200-239 → Borderline
≥240 → High
Determining Cholesterol Goal
(LDL!)
Look at JNC 7 Risk Factors
Cigarette smoking
Hypertension (BP ≥140/90 or on anti-
hypertensives)
Low HDL cholesterol (< 40 mg/dL)
Family History of premature coronary heart
disease (CHD) (CHD in first-degree male relative
<55 or CHD in first-degree female relative < 65)
Age (men ≥ 45, women ≥ 55)
Determining Goal LDL
CHD and CHD Risk Equivalents:
Peripheral Vascular Disease
Cerebral Vascular Accident
Diabetes Mellitus
LDL Goals
0-1 Risk Factors:
LDL goal is 160
If LDL ≥ 160: Initiate TLC (therapeutic lifestyle changes)
If LDL ≥ 190: Initiate pharmaceutical treatment
2 + Risk Factors
LDL goal is 130
If LDL ≥ 130: Initiate TLC
If LDL ≥ 160: Initiate pharmaceutical treatment
CHD or CHD Risk Equivalent
LDL goal is 100 (or 70)
If LDL ≥ 100: Initiate TLC and pharmaceutical treatment
Treatment of Hyperlipidemia
Lifestyle modification
Low-cholesterol diet
Exercise
Medications for Hyperlipidemia
Drug Class Agents Effects (% change) Side Effects
HMG CoA reductase Lovastatin LDL (18-55), HDL (5-15) Myopathy, increased liver
inhibitors Pravastatin Triglycerides (7-30) enzymes
Cholesterol Ezetimibe LDL( 14-18), HDL (1-3) Headache, GI distress
absorption inhibitor Triglyceride (2)
Nicotinic Acid LDL (15-30), HDL (15-35) Flushing, Hyperglycemia,
Triglyceride (20-50) Hyperuricemia, GI distress,
hepatotoxicity
Fibric Acids Gemfibrozil LDL (5-20), HDL (10-20) Dyspepsia, gallstones,
Fenofibrate Triglyceride (20-50) myopathy
Bile Acid Cholestyramine LDL GI distress, constipation,
sequestrants HDL decreased absorption of
other drugs
No change in triglycerides
Case # 1
A 55-year-old woman without symptoms of CAD
seeks assessment and advice for routine health
maintenance. Her blood pressure is 135/85 mm
Hg. She does not smoke or have diabetes and
has been postmenopausal for 3 years. Her BMI is
24. Lipoprotein analysis shows a total cholesterol
level of 240 mg/dL, an HDL level of 55 mg/dL, a
triglyceride level of 85 mg/dL and a LDL level is
180 mg/dL. The patient has no family history of
premature CAD.
Case # 1 (cont.)
What is the goal LDL in this woman?
What would you do if exercise/diet change
do not improve cholesterol after 3 months?
How would your management change if
she complained of claudication with
walking?
Case # 2
A 40- year-old man without significant past
medical history comes in for a routine annual
exam. He has no complaints but is worried
because his father had a “heart attack” at the age
of 45. He is a current smoker and has a 23-pack
year history of tobacco use. A fasting lipid panel
reveals a LDL 170 mg/dL and an HDL of 35
mg/dL. Serum Triglycerides were 140 mg/dL.
Serum chemistries including liver panel are all
normal.
Case # 2 (cont.)
What is this patient’s goal LDL?
Would you start medication, and if so,
what?
Case # 3
A 65 year-old woman with medical history of Type
II diabetes, obesity, and hypertension comes to
your office for the first time. She has been told her
cholesterol was elevated in the past and states
that she has been following a “low cholesterol diet”
for the past 6 months after seeing a dietician. She
had a normal exercise stress test last year prior to
knee replacement surgery and has never had
symptoms of CHD. A fasting lipid profile was
performed and revealed a LDL 130, HDL 30 and a
total triglyceride of 300. Her Hgba1c is 6.5%.
Case # 3 (cont.)
What is this patient’s goal LDL?
What medication would you consider
starting in this patient?
What labs would you want to monitor in this
patient?
Вам также может понравиться
- Guide to Hyperlipidemia (39Документ22 страницыGuide to Hyperlipidemia (39Faisal AhmedОценок пока нет
- Guide to Hyperlipidemia (39Документ22 страницыGuide to Hyperlipidemia (39Ritha WidyaОценок пока нет
- Guide to Hyperlipidemia (39Документ22 страницыGuide to Hyperlipidemia (39Febrina SusilawatiОценок пока нет
- Shelly HyperlipidemiaДокумент22 страницыShelly Hyperlipidemiaale marilОценок пока нет
- Hyperlipidemia 1Документ32 страницыHyperlipidemia 1Binita ShakyaОценок пока нет
- HyperlipidemiaДокумент33 страницыHyperlipidemiaHimaОценок пока нет
- Health and Nutrition: HyperlipidemiaДокумент20 страницHealth and Nutrition: HyperlipidemiaRinoy R BhagoraОценок пока нет
- 23 HyperlipidemiaДокумент85 страниц23 HyperlipidemiaIhab MoustafaОценок пока нет
- Hyperlipidemia: Center of Post Graduate Studies in Family MedicineДокумент85 страницHyperlipidemia: Center of Post Graduate Studies in Family MedicineShimelis MekitОценок пока нет
- Lipid Biokimia Semester 2Документ93 страницыLipid Biokimia Semester 2Anonymous oyAUZoCeyОценок пока нет
- Hyperlipidemia: Understanding High Cholesterol and How to Lower ItДокумент25 страницHyperlipidemia: Understanding High Cholesterol and How to Lower ItMarbungaran Putra GalinggingОценок пока нет
- Lipid ProfileДокумент2 страницыLipid ProfileFadia SharminОценок пока нет
- Dyslipidemia 2008Документ80 страницDyslipidemia 2008Pucca' JernyОценок пока нет
- Lipoprotein Tests: Cholesterol (140-199 MG/DL)Документ3 страницыLipoprotein Tests: Cholesterol (140-199 MG/DL)imperiouxxОценок пока нет
- Dyslipidemia: Signs and SymptomsДокумент24 страницыDyslipidemia: Signs and Symptomschrissanto chandraОценок пока нет
- Labs in DyslipedemiaДокумент38 страницLabs in DyslipedemiaMohiedine AbouljoudОценок пока нет
- The Complete Guide to High Cholesterol: Symptoms, Risks, Treatments & CuresОт EverandThe Complete Guide to High Cholesterol: Symptoms, Risks, Treatments & CuresОценок пока нет
- Chapter 8 Dyslipidemia: Understanding Cholesterol Levels and RisksДокумент10 страницChapter 8 Dyslipidemia: Understanding Cholesterol Levels and RisksFriska tampuboLonОценок пока нет
- Fact Pro CholesterolДокумент6 страницFact Pro CholesterolawepzreezyОценок пока нет
- High Cholesterol: Food & Nutrition IДокумент12 страницHigh Cholesterol: Food & Nutrition IAfnanОценок пока нет
- Dyslipidemia Harper CHOДокумент37 страницDyslipidemia Harper CHOC Hendra WijayaОценок пока нет
- Lipid Profile: by Micheal and ChristianДокумент15 страницLipid Profile: by Micheal and ChristianMichealОценок пока нет
- Lipid Profile TestДокумент2 страницыLipid Profile TestPrateek KanadeОценок пока нет
- Keys To Lower: CholesterolДокумент21 страницаKeys To Lower: CholesterolAbdulkareem AlBabtainОценок пока нет
- HyperlipidemiasДокумент47 страницHyperlipidemiasPushpa Paul 2021665649Оценок пока нет
- High CholesterolДокумент31 страницаHigh Cholesterolashoku2100% (1)
- HDL (Good) Cholesterol - HDL Stands For High-Density Lipoproteins. These AreДокумент10 страницHDL (Good) Cholesterol - HDL Stands For High-Density Lipoproteins. These ArenaliniОценок пока нет
- HYPERLIPIDEMIAДокумент33 страницыHYPERLIPIDEMIAatiqullah tarmiziОценок пока нет
- HyperlipidemiasДокумент62 страницыHyperlipidemiasIsrat Jahan Surovy 2225400672Оценок пока нет
- Dyslipidemia 2023Документ39 страницDyslipidemia 2023medt80Оценок пока нет
- Understanding Cholesterol Levels and Risks: A Guide to Lipid ProfilesДокумент48 страницUnderstanding Cholesterol Levels and Risks: A Guide to Lipid ProfilesAnonymous o3Q3QXEОценок пока нет
- Management of HyperlipidemiaДокумент39 страницManagement of HyperlipidemiaRajgopal100% (2)
- A Hyper - Emia A A PseudohyponatremiaДокумент14 страницA Hyper - Emia A A PseudohyponatremiaSrinivas PolikepatiОценок пока нет
- Cholestrol Group AДокумент23 страницыCholestrol Group Aapi-303116697Оценок пока нет
- Cholesterol Testing and ResultsДокумент3 страницыCholesterol Testing and ResultsJose OliverosОценок пока нет
- 4.investigations of Serum LipidsДокумент7 страниц4.investigations of Serum LipidsMV ProductionОценок пока нет
- Dyslipidemia Diagnosis and TreatmentДокумент5 страницDyslipidemia Diagnosis and TreatmentEisuke HondouОценок пока нет
- High triglycerides natural support strategiesДокумент42 страницыHigh triglycerides natural support strategiesPaul Ioan Popescu100% (1)
- Understanding LDL and HDL Cholesterol LevelsДокумент16 страницUnderstanding LDL and HDL Cholesterol LevelsaakashtrivediОценок пока нет
- Management Strategies For Patients/Clients: DyslipidemiaДокумент7 страницManagement Strategies For Patients/Clients: DyslipidemiaminkyaoОценок пока нет
- Tangier DiseaseДокумент13 страницTangier DiseaseSyifa NawwarОценок пока нет
- Med 4 Lipedemias and Ischemic Heart DiseaseДокумент47 страницMed 4 Lipedemias and Ischemic Heart DiseaseNathanОценок пока нет
- DyslipidaemiaДокумент34 страницыDyslipidaemiaMusfique RashidОценок пока нет
- AtherosclerosisДокумент29 страницAtherosclerosisneeraj banaОценок пока нет
- Lipid Profile, Ischemic Heart Disease and Its Risk Factors: Muhammad Asif Shaheen Lecturer Pathology KEMU, LahoreДокумент38 страницLipid Profile, Ischemic Heart Disease and Its Risk Factors: Muhammad Asif Shaheen Lecturer Pathology KEMU, LahoreRimsha MustafaОценок пока нет
- Medical Nutrition Therapy in Cardiovascular DiseaseДокумент93 страницыMedical Nutrition Therapy in Cardiovascular DiseasesariОценок пока нет
- Screening and Management of DyslipidemiaДокумент16 страницScreening and Management of DyslipidemiaSakina GhaziОценок пока нет
- Treatment of Hyperlipidemias: Pharmacology TeamДокумент53 страницыTreatment of Hyperlipidemias: Pharmacology TeamZaina Masri100% (1)
- CholesterolДокумент10 страницCholesterolapi-273977307Оценок пока нет
- HIPERKOLESTEROLДокумент16 страницHIPERKOLESTEROLAnonymous 1jCVqQuОценок пока нет
- Managing Hyperlipidemia in a 56-Year-Old Male PatientДокумент11 страницManaging Hyperlipidemia in a 56-Year-Old Male Patientabdul basithОценок пока нет
- Coronary Artery DiseaseДокумент46 страницCoronary Artery DiseasemrwaseeОценок пока нет
- High CholesterolДокумент31 страницаHigh CholesterolDini ZakiaОценок пока нет
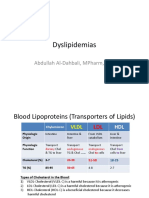
- Dyslipidemias: Abdullah Al-Dahbali, Mpharm, PHDДокумент15 страницDyslipidemias: Abdullah Al-Dahbali, Mpharm, PHDعزالدين الطيارОценок пока нет
- Coronary Artery DiseaseДокумент46 страницCoronary Artery DiseaseRameez ShamounОценок пока нет
- Chapter-Xi Lipid Profile TestsДокумент4 страницыChapter-Xi Lipid Profile TestssabrinaОценок пока нет
- Blood Lipid MeasurementДокумент2 страницыBlood Lipid MeasurementSharif M Mizanur RahmanОценок пока нет
- Understanding Your Cholesterol Report: What the Numbers MeanДокумент3 страницыUnderstanding Your Cholesterol Report: What the Numbers MeanBuddhika NawagamuwaОценок пока нет
- Eat Well Live Well with High Cholesterol: Low-Cholesterol Recipes and TipsОт EverandEat Well Live Well with High Cholesterol: Low-Cholesterol Recipes and TipsОценок пока нет
- The No-hoax Cholesterol Management Book: Bust the cholesterol myth, get clarity to get natural protection for life by knowing how to control & lower down cholesterol via medicine, exercise & dietОт EverandThe No-hoax Cholesterol Management Book: Bust the cholesterol myth, get clarity to get natural protection for life by knowing how to control & lower down cholesterol via medicine, exercise & dietРейтинг: 5 из 5 звезд5/5 (1)
- Cynara Scolymus ArtichokeДокумент8 страницCynara Scolymus Artichokeplanet_renОценок пока нет
- CS1 AntibioticsДокумент4 страницыCS1 AntibioticsTaraKyleUyОценок пока нет
- Pediatric Nursing Care PlanДокумент18 страницPediatric Nursing Care PlanRo Vin100% (2)
- Clinical Pharmacy: Pathophysiology and Pharmacotherapy of Congestive Heart FailureДокумент89 страницClinical Pharmacy: Pathophysiology and Pharmacotherapy of Congestive Heart FailureMuhammad Mustafa Ijaz100% (3)
- Micro K (Potassium Chloride)Документ2 страницыMicro K (Potassium Chloride)EОценок пока нет
- Senior Care Plan (: For Ages 61-100 Yrs Old)Документ7 страницSenior Care Plan (: For Ages 61-100 Yrs Old)Clarissa RefugioОценок пока нет
- Pediatric Nursing QuestionsДокумент8 страницPediatric Nursing QuestionsLouie A. Gallego50% (2)
- Scientific PapersДокумент98 страницScientific PapersZack MarksОценок пока нет
- PHYSIOLOGY OF RED BLOOD CELLSДокумент7 страницPHYSIOLOGY OF RED BLOOD CELLSRoderick PalattaoОценок пока нет
- Comparison of Ef Ficacy and Safety of Atorvastatin 5% Lotion and Betamethasone 0.1% Lotion in The Treatment of Scalp Seborrheic DermatitisДокумент9 страницComparison of Ef Ficacy and Safety of Atorvastatin 5% Lotion and Betamethasone 0.1% Lotion in The Treatment of Scalp Seborrheic DermatitisJody Fajar HibatullahОценок пока нет
- Malabsorption and Elimination DisordersДокумент120 страницMalabsorption and Elimination DisordersBeBs jai SelasorОценок пока нет
- 1 كتب دكتور علام باطنه General & Cardio.whiteKnightLoveДокумент111 страниц1 كتب دكتور علام باطنه General & Cardio.whiteKnightLoveNour ShăbanОценок пока нет
- Anasarca - StatPearls - NCBI BookshelfДокумент5 страницAnasarca - StatPearls - NCBI Bookshelfemail lombaОценок пока нет
- Karoshi PDFДокумент6 страницKaroshi PDFJuanito MaravillasОценок пока нет
- File 18588Документ4 страницыFile 18588Mohammed MuthanaОценок пока нет
- Augenblickdiagnos Campbell1998 PDFДокумент8 страницAugenblickdiagnos Campbell1998 PDFFrancoОценок пока нет
- Hema 5 - Erythrocyte MorphologyДокумент42 страницыHema 5 - Erythrocyte MorphologySincerely PascualОценок пока нет
- Vasculitis SyndromesДокумент9 страницVasculitis Syndromesapi-3704562Оценок пока нет
- ICD10Документ263 страницыICD10Bharath HollaОценок пока нет
- Maturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementДокумент10 страницMaturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementatikahanifahОценок пока нет
- Surgical Pathology of Liver TumorsДокумент480 страницSurgical Pathology of Liver TumorsGeorgiana BuhociОценок пока нет
- (Christopher Donald Frith) The Cognitive Neuropsyc (BookFi) PDFДокумент91 страница(Christopher Donald Frith) The Cognitive Neuropsyc (BookFi) PDFVinoth Babu100% (1)
- MIB - Internal Medicine 2 Semester 8 Updated March 2021Документ26 страницMIB - Internal Medicine 2 Semester 8 Updated March 2021Kavin VarmaОценок пока нет
- Тopic 2. Review of individual body partsДокумент13 страницТopic 2. Review of individual body partslayla kambalaОценок пока нет
- Principles of Pediatrics by Adeleke: Key ConceptsДокумент17 страницPrinciples of Pediatrics by Adeleke: Key ConceptsTianah davis50% (4)
- Oily Skin Case StudyДокумент4 страницыOily Skin Case StudyLionel YdeОценок пока нет
- UNAS 59th (NOV 2020) FIXДокумент23 страницыUNAS 59th (NOV 2020) FIXmhariskurniawanОценок пока нет
- Ayurvedic Diabetes CureДокумент12 страницAyurvedic Diabetes Curepshashi71% (7)
- Seminar On Rhuematic Heart DiseaseДокумент16 страницSeminar On Rhuematic Heart Diseasenaga maniОценок пока нет
- Thyroid Case ProformaДокумент2 страницыThyroid Case ProformaSneha NaulakhaОценок пока нет