Академический Документы
Профессиональный Документы
Культура Документы
Respiratory Diseases WK 5
Загружено:
Sharmaigne Bianca NecorИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Respiratory Diseases WK 5
Загружено:
Sharmaigne Bianca NecorАвторское право:
Доступные форматы
y
is the inflammation of the lung parenchyma (terminal bronchioles, respiratory bronchioles, alveolar ducts, alveolar sac, and alveoli) it is classified according to its causative agent; the incubation period depends on what type of microorganism caused the disease;
pneumonia usually arises from endogenous microflora of the person whose resistance have been altered or from aspiration of oropharyngeal secretions; patients with pneumonia may have an underlying infection that impairs host defense;
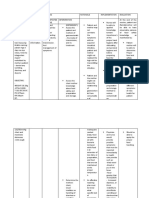
Bacterial Pneumonia
x Streptococcus pneumoniae x Staphylococcus aureus x Gram-negative Bacteria Klebsiella, Pseudomonas, or Escherichia; x Hemophilus influenzae x Atypical Pneumonia walking pneumonia x Legionella pneumophila x Mycoplasma pneumoniae x Chlamydia trachomatis
Viral Pneumonia
x Influenza viruses x Parainfluenza x Adenoviruses
Fungal Pneumonia
x Aspergillus fumigatus x Pneumocystis carinii AIDS patients
Mode of Transmission:
Inhalation of respiratory secretions from
an infected individual; Aspiration of oropharyngeal secretions; Thru the bloodstream; From direct spread as a result of surgery or trauma;
Clinical Manifestations:
Sudden onset of fever, high-grade with chills; Cough, productive; Dyspnea; Pleuritic chest pain aggravated by coughing or breathing; Tachypnea accompanied by grunting, nasal flaring, use of accessory muscles and fatigue; Rapid, bounding pulse;
Diagnostic Evaluation:
CBC Chest X-ray to show presence of pneumonic infiltrates and the extent of pneumonia. Sputum Grams stain - may indicate offending microorganism; Sputum culture and sensitivity may also confirm offending microorganism; Blood culture to confirm the presence of bacterial pneumonia; Immunologic test detecting microbial antigens in serum, sputum, and urine.
Medical Management:
Antimicrobial therapy x Depends on laboratory identification of causative agents and its sensitivity; x For Bacterial pneumonia:
x x x x x Penicillin Cefuroxime Ceftriaxone Cotrimoxazole Azithromycin
x For Viral Pneumonia x Most of the time it is self-limiting. x Symptomatic and supportive management.
Oxygen therapy Mucolytic and other cough medicines Bronchodilators Steroid therapy
Nursing Diagnosis:
Impaired gas exchange Ineffective airway clearance
Nursing Interventions:
Assess px for cyanosis, dyspnea, hypoxia, and confusion; Administer oxygen as indicated at 1-2 L/min. Isolate the client. Put client is semi-Fowlers position. Encourage the px to cough out secretions. Encourage increase fluid intake. Employ chest wall percussion and postural drainage. Auscultate chest for crackles and rhonchi. Mobilize client even on bed to improve secretion clearance.
Complications:
Pleural effusion parapneumonic effusion Cardiovascular collapse especially from
gram (-) bacteria/sepsis; Superinfection Delirium due to cerebral hypoxia; Atelectasis
is a chronic bacterial infection characterized by granuloma formation, necrosis, and calcification of involved tissues; one of the leading cause of morbidity and mortality in the Philippines and other developing countries. fairly common among low-income, congested families;
approximately 10% (5 - 14%) of cases are ASYMPTOMATIC;
can be:
Minimal slight lesions without demonstrable excavation and confined to the apex; Moderately Advanced cavities less than 4 cm involving one or both lungs; Far Advanced lesions more extensive than moderately advanced TB;
Causative Agent: Mycobacterium tuberculosis
x acid-fast bacilli, aerobic;
IP:
3 8 weeks;
Mode of Transmission;
Nasopharyngeal secretions Drinking of infected cows milk Droplet nuclei infection
TB Classification according to ATS:
Class 0 no TB exposure; no infection; (-) PPD; Class 1 (+) exposure; no infection; (-) PPD; Class 2 (+) exposure; (+) PPD; no symptoms;
x Recent or actual TB infection;
Class 3 (+) exposure; (+) PPD; (+) symptoms; (+) CXR;
x Active TB;
Class 4 (+) exposure; (+) PPD; no active disease; (+) CXR;
x Previous PTB disease;
Class 5 (+) exposure; (+) PPD; (+) CXR; equivocal findings;
x PTB Suspect;
Multiple Drug-Resistance Tuberculosis (MDRTB) suspect in PTB class 3 patients who are still sputum smear or sputum culture positive (+) despite 3 months of adequate treatment;
Clinical Manifestations:
fever, low-grade, late afternoon or early evening; chills anorexia weight loss chronic cough more than two weeks; nocturnal sweating chest and back pains dyspnea and hemoptysis
Diagnostic Examinations:
Chest X-ray (PA - lateral and apicolordotic view) Sputum AFB 3 consecutive mornings; to identify if the client is communicable;
x Tell client not to eat or brush before collecting sputum. x Client may gurgle tap water. x If client cannot expectorate, may nebulizer with PNSS.
Bronchoscopy Mantoux test or PPD; exposure to TB; Mycobacterium TB Culture confirmatory; Liver Function Test AST and ALT;
1. First-line Medications -
RIPES
RIFAMPICIN (RIF) taken WITH food to prevent GI upset; x causes hepatotoxicity (reddish-orange urine) ISONIAZID (INH) taken on an EMPTY stomach for maximum absorption; x causes PERIPHERAL NEUROPATHY (char by numbness and tingling sensation of hands and feet) x given with PYRIDOXINE (Vit. B6); x Avoid thyramine containing foods because they may cause reaction PYRAZINAMIDE (PZA) causes hepatotoxicity and hyperuricemia; x protect drug from light; ETHAMBUTOL (EMB) causes OPTIC NEURITIS characterized by blurring of vision; x not given in children less than 6 years old; x Administer with food STREPTOMYCIN must weigh px daily and monitor kidney function; x causes OTOTOXICITY and NEPHROTOXICITY; x can be given to children less than 6 y/o; x Obtain baseline audiometric test and repeat every 1 to 2 monyhs
Second-line Drugs
Amikacin Capreomycin Ciprofloxacin Cycloserine Ofloxacin Terizidone
Nursing Interventions:
Isolate client for TWO WEEKS at the start of ANTI-TB drugs. Provide px with adequate rest periods; Promote adequate nutrition Advise to cover nose and mouth when sneezing and coughing; Provide frequent oral hygiene and hand washing; Monitor intake of medications;
Factors that contribute to the development of the disease:
Poverty Overcrowding Malnutrition Vitamin deficiencies (A, D, C) Decrease resistance due to existing infections (that threatens their immune system). Children below 5yrs old who are prone to infections due to factors found above.
Acute viral infection affecting the respiratory system Etiologic agent: myxoviruses, types A, Aprime, B, C IP 24-48 hours
POC up to 5th day of illness in children
MOT Airborne Direct contact droplet
Manifestations y Chilly sensation y Hyperpyrexia y Malaise y Sore throat y Coryza y Rhinorrhea y Myalgia y headache
Diagnostic procedures Blood exams Oropharyngeal swabbing
Management No specific treatment Symptomatic rest
Preventive measure Immunization Avoidance of crowded places
y is
an acute contagious viral infection in the new millennium that originate in Guandong Province of China; coined by Dr. Carlo Urbani (WHO) last 2002;
y term
y it
causes severe form of atypical pneumonia;
only has a 5% mortality rate in all cases found around the world; significant history of travel to affected areas such as Guandong, China; Hong Kong; Taiwan, and Singapore; at risk are individuals that are in close contact with a SARS patient (health workers, family members, care givers, classmates)
Causative Agent: SARS-corona virus.
x a variant of the common cold coronavirus x Virus survival outside body: x 3 hours dry environment. x 6 hours moist setting. x Can be killed by exposure to sunlight. x Mutates easily.
IP: 1 - 13 days (ave. 2 5 days)
Mode of Transmission:
Airborne transmission Indirect contact with inanimate objects contaminated with nasopharyngeal and respiratory secretions;
Clinical Manifestations:
Fever, moderate- to- high-grade fever. Chills. Flu-like manifestations. Cough, productive or non-productive. Sudden episode of dyspnea.
Diagnostic Examination
CXR shows atypical form of pneumonia; CBC leucopenia and lymphopenia; Elevated lactate dehydrogenase. Elevated liver function test (AST and ALT) Viral Culture; Immunologic Test identify antibodies against the virus.
Medical Management:
Supportive management such as
ventilatory support; Use of Anti-viral agents, steroids, and large doses of antibiotics are controversial;
Nursing Diagnosis:
Impaired airway clearance Ineffective breathing pattern High risk for injury: Death
Nursing Interventions:
ISOLATE!!! Practice barrier method. Use complete PPE when caring for the patient; Monitor the patient for signs of respiratory distress; Advise relatives or anybody that were in close contact with the patient to undergo observation and quarantine; Educate the px and family about hand washing and handling linens and clothing properly.
is an acute contagious bacterial infection characterized by paroxysms of repeated cough and ends in a whooping sound; common in children LESS THAN TWO YEARS OLD. Causative Agent: Bordetella pertussis IP: 7 21 days;
y y
Mode of Transmission:
Direct contact by airborne transmission Indirect contact thru nasopharyngeal
secretions;
Clinical Manifestations:
Invasive Stage or catarrhal stage; x 7 14 days; x patient is highly contagious; x Fever x Watery eyes and sneezing x Nocturnal coughing x Restlessness or irritable
Spasmodic Stage 4 12 weeks;
x Forceful successive coughing with peculiar crowing sound or whoop; x 5 20 coughing; x Protrusion of tongue and eyeballs during coughing; x Swollen face and neck;
Convalescent Stage
x symptoms subsides;
Diagnostic Examination:
Cough plate or agar plate;
Medical Management:
Antibiotics Penicillin or Erythromycin; O2 inhalation Prevent convulsions
Nursing Interventions:
ISOLATE the client!!! provide a quiet and non-stimulating
environment; complete bed rest; small frequent feeding Prevention: x DPT vaccination;
is an infestation of the skin produced by BURROWING action of the parasite mite resulting in irritation and the formation of vesicles or pustules;
common in individuals living in areas of poverty where cleanliness is lacking;
Causative Agent: Sarcoptes scabiei
Mode of Transmission:
Skin contact with an infected person; Indirect contact thru soiled bed linens and
clothing;
Clinical Manifestations:
Intense itchiness especially at night; Sites:
x Interdigital areas x Flexor surface of the wrist and palms; x Nipples x Umbilicus x Axillary folds x Groin or gluteal folds x Penis and scrotum
Diagnostic Examination:
Presence on skin of female mites,
ova, and feces upon skin biopsy or scraping;
Medical Management:
Permethrin 5% cream apply on the skin
below the neck; stay for at least 8 hours. Lindane solution (Kwell) for bathing; Crotamiton (Eurax) ointment; Anti-histamines to reduce itchiness.
Nursing Interventions:
Boiling of linens and clothes; Encourage to change clothing and bed
linen frequently Warm shower bath to remove scaling debris or crusts;
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Chapter IДокумент19 страницChapter ISharmaigne Bianca NecorОценок пока нет
- NRESДокумент1 страницаNRESSharmaigne Bianca NecorОценок пока нет
- Scope and DelimitationДокумент2 страницыScope and DelimitationSharmaigne Bianca Necor100% (1)
- NCP 2Документ1 страницаNCP 2Sharmaigne Bianca NecorОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- GW N2Документ2 страницыGW N2nikhilesh sharmaОценок пока нет
- Standard Operating ProcedureДокумент15 страницStandard Operating ProcedureAyman AliОценок пока нет
- Immunization EPI Huda 201212Документ5 страницImmunization EPI Huda 201212Aerish TupazОценок пока нет
- Dark AgesДокумент10 страницDark AgesIamee Moranta ApareceОценок пока нет
- Case Study Pneumonia PediaДокумент13 страницCase Study Pneumonia PediaAinurul FatehahОценок пока нет
- Aloe Vera EthanolicextractsofaloeveraДокумент8 страницAloe Vera EthanolicextractsofaloeveraBashaar HamdaanОценок пока нет
- Methisoprinol in The Treatment of Non-Bacterial PharyngitisДокумент3 страницыMethisoprinol in The Treatment of Non-Bacterial PharyngitisSalifah SafiraОценок пока нет
- F8DB F089:Fungal InfectionsДокумент6 страницF8DB F089:Fungal InfectionsPharmacist Ehab HammadОценок пока нет
- MalariaДокумент5 страницMalariaRina KhazarenОценок пока нет
- Examining RFK JRДокумент7 страницExamining RFK JRMarieОценок пока нет
- Edgcse Aap Sb5i Homework2Документ1 страницаEdgcse Aap Sb5i Homework2Martina La Rocca Márquez Year 10Оценок пока нет
- NCP For GastroenteritisДокумент8 страницNCP For GastroenteritisNur SanaaniОценок пока нет
- NCM 112 Care of Clients With ProblemsДокумент3 страницыNCM 112 Care of Clients With Problems2C - Michaela Shenna DelfinОценок пока нет
- Summary of Infectious DiseasesДокумент415 страницSummary of Infectious DiseasesAlston Foods BVОценок пока нет
- SACMC - 19052020 - Slides For MoHmediabriefingДокумент21 страницаSACMC - 19052020 - Slides For MoHmediabriefingBranko Brkic93% (15)
- Update Stock PT KMD 14-6Документ46 страницUpdate Stock PT KMD 14-6rio1995Оценок пока нет
- Infective EndocarditisДокумент3 страницыInfective EndocarditisRechelle CabagingОценок пока нет
- Essay HivДокумент2 страницыEssay HivPopoo KyoОценок пока нет
- Neonatal Pneumonia in Developing Countries: Arch. Dis. Child. Fetal Neonatal EdДокумент10 страницNeonatal Pneumonia in Developing Countries: Arch. Dis. Child. Fetal Neonatal EdadiОценок пока нет
- Tanauan City Integrated High School Trapiche 1, Tanauan City, Batangas Health Declaration FormДокумент4 страницыTanauan City Integrated High School Trapiche 1, Tanauan City, Batangas Health Declaration FormKurt VillaОценок пока нет
- Thelma ImmunizationДокумент51 страницаThelma Immunizationclement johnОценок пока нет
- ABO Discrepancies QuizДокумент4 страницыABO Discrepancies Quizwe445Оценок пока нет
- DengueДокумент4 страницыDengueNallely LeónОценок пока нет
- Chapter 4 Social Pharmacy Introduction To Microbiology and Common NoteskartsДокумент6 страницChapter 4 Social Pharmacy Introduction To Microbiology and Common NoteskartsSushovan AshОценок пока нет
- Draft Articel KKN Agatha Dwi Natasya RevДокумент8 страницDraft Articel KKN Agatha Dwi Natasya RevAgatha Dwi NatasyaОценок пока нет
- Vaginal Discharge: By: Lisa Anggraeni Rizki FadillahДокумент12 страницVaginal Discharge: By: Lisa Anggraeni Rizki FadillahRizkifadillahОценок пока нет
- Dengue ReportДокумент48 страницDengue ReportRuthy SegoviaОценок пока нет
- Pathology Test Performed: Assay InterpretationДокумент1 страницаPathology Test Performed: Assay InterpretationjyzrОценок пока нет
- EncephalitisДокумент7 страницEncephalitisWiljohn de la CruzОценок пока нет
- 6075 Article Text 42975 1 10 20220630Документ14 страниц6075 Article Text 42975 1 10 20220630Laborat MenurОценок пока нет