Академический Документы
Профессиональный Документы
Культура Документы
RH Incompatibility
Загружено:
Serafin Dimalaluan IIIИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
RH Incompatibility
Загружено:
Serafin Dimalaluan IIIАвторское право:
Доступные форматы
Prepared by : Dimalaluan, Serafin III
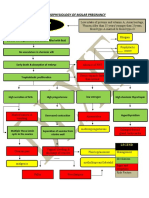
The Rh factor (ie, Rhesus factor) is a red blood cell surface antigen that was named after the monkeys in which it was first discovered. Rh incompatibility, also known as Rh disease, is a condition that occurs when a woman with Rh-negative blood type is exposed to Rh-positive blood cells, leading to the development of Rh antibodies.
Rh incompatibility can occur by 2 main mechanisms. The most common type occurs when an Rhnegative pregnant mother is exposed to Rh-positive fetal red blood cells secondary to fetomaternal hemorrhage during the course of pregnancy from spontaneous or induced abortion, trauma,invasive obstetric procedures, or normal delivery. Rh incompatibility can also occur when an Rh-negative female receives an Rh-positive blood transfusion. In part, this is the reason that blood banks prefer using blood type "O negative" or "type O, Rh negative," as the universal donor type in emergency situations when there is no time to type and crossmatch blood.
The most common cause of Rh incompatibility is exposure from an Rh-negative mother by Rhpositive fetal blood during pregnancy or delivery. As a consequence, blood from the fetal circulation may leak into the maternal circulation, and, after a significant exposure, sensitization occurs leading to maternal antibody production against the foreign Rh antigen. Once produced, maternal Rh immunoglobulin G (IgG) antibodies may cross freely from the placenta to the fetal circulation, where they form antigen-antibody complexes with Rh-positive fetal erythrocytes and eventually are destroyed, resulting in a fetal alloimmune-induced hemolytic anemia. Although the Rh blood group systems consist of several antigens (eg, D, C, c, E, e), the D antigen is the most immunogenic; therefore, it most commonly is involved in Rh incompatibility.
During pregnancy, red blood cells from the fetus can get
into the mother's bloodstream as she nourishes her child through the placenta. If the mother is Rh-negative, her immune system treats the Rh-positive fetal cells as if they were a foreign substance and makes antibodies against the fetal blood cells. These anti-Rh antibodies may cross the placenta into the developing baby, where they destroy the baby's circulating red blood cells. When red blood cells are broken down, they makebilirubin, which causes an infant to become yellow (jaundiced). The level of bilirubin in the infant's bloodstream may range from mild to dangerously high. First-born infants are often not affected -- unless the mother has had previous miscarriages or abortions, which could have sensitized her system -- as it takes time for the mother to develop antibodies against the fetal blood. However, second children who are also Rhpositive may be harmed. Rh incompatibility develops only when the mother is Rhnegative and the infant is Rh-positive. This problem has become uncommon in the U.S. and other places that provide good prenatal care. Special immune globulins, called RhoGAM, are now used to prevent RH incompatibility.
Factors that influence an Rh-negative pregnant female's chances of developing Rh incompatibility include the following: Ectopic pregnancy Placenta previa Placental abruption Abdominal/pelvic trauma In utero fetal death Any invasive obstetric procedure (eg, amniocentesis) Lack of prenatal care Spontaneous abortion
Signs
and symptoms
Jaundice Motor
and mental retardation Polyhydramnios (excess amniotic fluid)
Diagnostic Antibody
test :
screening Blood test (cbc) Amniocentesis Positive direct coombs test
Treatment Rh
immune globulin Blood transfusion (for hemolytic anemia) RHOgam Phototherapy using bilirubin lights
Вам также может понравиться
- RH IncompatibilityДокумент14 страницRH IncompatibilityMark Terence Padua AbrenicaОценок пока нет
- RH Incompatibil TY: What Is RH Incompatibility?Документ15 страницRH Incompatibil TY: What Is RH Incompatibility?Jannah Marie A. DimaporoОценок пока нет
- Pathophysiology of Erythroblastosis Fetalis - RH IsoimmunizationДокумент1 страницаPathophysiology of Erythroblastosis Fetalis - RH IsoimmunizationRalph Delos SantosОценок пока нет
- Retained Placental FragmentsДокумент9 страницRetained Placental FragmentsHannah Laput100% (2)
- Family Health ProfileДокумент11 страницFamily Health ProfileCharm RoweОценок пока нет
- Rh incompatibility causes and preventionДокумент10 страницRh incompatibility causes and preventionVernie Dinglasa GeligОценок пока нет
- Cervical IncompetenceДокумент30 страницCervical IncompetenceSignor ArasОценок пока нет
- PLacenta PreviaДокумент10 страницPLacenta Previaeyestrain_ajpn5001Оценок пока нет
- Pre EclampsiaДокумент13 страницPre EclampsiaEniamrahs DnalonОценок пока нет
- Chapter 24: Nursing Care of A Family During A Surgical Intervention For BirthДокумент22 страницыChapter 24: Nursing Care of A Family During A Surgical Intervention For BirthAlyssaGrandeMontimorОценок пока нет
- Senile Cataract (Age-Related Cataract) - Practice Essentials, Background, PathophysiologyДокумент5 страницSenile Cataract (Age-Related Cataract) - Practice Essentials, Background, PathophysiologyAhmad FahroziОценок пока нет
- Case StudyДокумент5 страницCase StudyMoath MahmoudОценок пока нет
- Placenta Abruptio - Topic OverviewДокумент8 страницPlacenta Abruptio - Topic OverviewLei AbellarОценок пока нет
- Bleeding During Pregnancy Care PlanДокумент17 страницBleeding During Pregnancy Care PlanLizcelle Bihasa86% (7)
- Pathophysiology of Gestational DMДокумент3 страницыPathophysiology of Gestational DMAnonymous GtR96jCОценок пока нет
- NCP NecДокумент1 страницаNCP NecandikaisnaeniОценок пока нет
- NCP - Diabetes Mellitus Prepregnancy/GestationalДокумент13 страницNCP - Diabetes Mellitus Prepregnancy/GestationalClaudine Christophe100% (1)
- RH Incompatibility - RupeshДокумент4 страницыRH Incompatibility - Rupeshrupesh_mamidi100% (2)
- Newborn Hypothermia and Hyperthermia (Final Copy)Документ30 страницNewborn Hypothermia and Hyperthermia (Final Copy)Shizuka Marycris Amane67% (3)
- Sarcoma NCPДокумент8 страницSarcoma NCPginosanОценок пока нет
- Anatomy and Physiology of PlacentaДокумент5 страницAnatomy and Physiology of PlacentaAdrianne Basa100% (1)
- Case Study Placenta Previa This Is It 1Документ71 страницаCase Study Placenta Previa This Is It 1Homework Ping100% (1)
- How to take iron supplements during pregnancyДокумент7 страницHow to take iron supplements during pregnancyjose godfreycОценок пока нет
- IMCI Sesion 5 - Malnutrition and AnemiaДокумент37 страницIMCI Sesion 5 - Malnutrition and Anemiasarguss14100% (4)
- Partial Mole or Complete Mole: Pathophysiology of Molar PregnancyДокумент1 страницаPartial Mole or Complete Mole: Pathophysiology of Molar PregnancyKristian Karl Bautista Kiw-isОценок пока нет
- Problem # 3: Threat of Cross Infection From A Communicable Disease CaseДокумент3 страницыProblem # 3: Threat of Cross Infection From A Communicable Disease CaseRolandОценок пока нет
- Indirect Inguinal Hernia FINALДокумент6 страницIndirect Inguinal Hernia FINALJonalyn TumanguilОценок пока нет
- Incompetent CervixДокумент5 страницIncompetent CervixNaidin Catherine De Guzman-Alcala100% (1)
- Pathophysiology of Hypersensitivity Type IIДокумент2 страницыPathophysiology of Hypersensitivity Type IItwin_smartyОценок пока нет
- C-Section Case StudyДокумент24 страницыC-Section Case StudyQieyla QilaОценок пока нет
- Case Report Tetralogy of Fallot-CompleteДокумент72 страницыCase Report Tetralogy of Fallot-CompleteMaydis stigmaОценок пока нет
- In Partial Fulfillment in Related Learning Experience Presented ToДокумент14 страницIn Partial Fulfillment in Related Learning Experience Presented ToFrances PerezОценок пока нет
- Jaundice NeonatalДокумент26 страницJaundice Neonatalhunk2662Оценок пока нет
- Newborn AssessmentДокумент9 страницNewborn Assessmentapi-237668254Оценок пока нет
- Preeclampsia, Severe, UncontrolledДокумент22 страницыPreeclampsia, Severe, UncontrolledLharra Cagulada-PostranoОценок пока нет
- UoB Nursing Students' Case Study on Normal Spontaneous Vaginal DeliveryДокумент21 страницаUoB Nursing Students' Case Study on Normal Spontaneous Vaginal DeliveryJaysellePuguonTabijeОценок пока нет
- Hemolytic Disease of NewbornДокумент15 страницHemolytic Disease of Newborncyphochilus100% (1)
- Premature Rupture of MembraneДокумент7 страницPremature Rupture of MembranedrommygreatОценок пока нет
- Acute Lymphocytic Leukemia Treatment PaperДокумент18 страницAcute Lymphocytic Leukemia Treatment Paperapi-282231236Оценок пока нет
- ABO Incompatibility in Newborns ExplainedДокумент9 страницABO Incompatibility in Newborns ExplainedJuli-anne Villarico AndresОценок пока нет
- Dysfunctional Labor DystociaДокумент8 страницDysfunctional Labor Dystociamardsz100% (2)
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationДокумент1 страницаNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyОценок пока нет
- Nursing Diagnosis For Ante Part Um, Um and PostДокумент10 страницNursing Diagnosis For Ante Part Um, Um and Postxtn218100% (13)
- Incomplete Abortion MINI CASE STUDY Group 3Документ23 страницыIncomplete Abortion MINI CASE STUDY Group 3Katrina TinapianОценок пока нет
- Neonatal Case 1 (Normal) - AGA Male Infant Born at 38 WeeksДокумент5 страницNeonatal Case 1 (Normal) - AGA Male Infant Born at 38 WeeksRexelle RamosОценок пока нет
- CP Ovarian Cyst Chap5Документ11 страницCP Ovarian Cyst Chap5Katherine 'Chingboo' Leonico LaudОценок пока нет
- Uterine AtonyДокумент3 страницыUterine AtonyArsheina Paradji100% (1)
- Cord Prolapse March 23Документ2 страницыCord Prolapse March 23Kathleen Vargas100% (1)
- NCP For FT, SGAДокумент7 страницNCP For FT, SGAJule Santoya80% (5)
- What Is Retained PlacentaДокумент7 страницWhat Is Retained PlacentaA Xiao Yhing TrancoОценок пока нет
- Date Cues Nursing Diagnosis Scientific Basis Goal of Care Nutsing Interventi ON Rationale EvaluationДокумент5 страницDate Cues Nursing Diagnosis Scientific Basis Goal of Care Nutsing Interventi ON Rationale EvaluationNathalie kate petallarОценок пока нет
- Myoma CaseДокумент111 страницMyoma Caseapi-1976296750% (2)
- Typology of Nursing Problems in Family Nursing PracticeДокумент17 страницTypology of Nursing Problems in Family Nursing PracticeAnonymous iG0DCOfОценок пока нет
- RH IncompatibilityДокумент6 страницRH IncompatibilityEly TaОценок пока нет
- Background: RH IncompatibilityДокумент8 страницBackground: RH IncompatibilityBrett StevensonОценок пока нет
- RH IncompatibilityДокумент7 страницRH IncompatibilityMichael CabiliОценок пока нет
- RH Incompatibility: Go ToДокумент4 страницыRH Incompatibility: Go ToFadhila AnasОценок пока нет
- RH DiseaseДокумент9 страницRH DiseaseYerra SukumalaОценок пока нет
- Pathophysiology: RH Disease (Also Known As RhesusДокумент3 страницыPathophysiology: RH Disease (Also Known As RhesusZum LopisОценок пока нет
- Maternal antibodies attack fetal red blood cells in HDNДокумент7 страницMaternal antibodies attack fetal red blood cells in HDNLara CarisaОценок пока нет
- MaternalДокумент347 страницMaternalJosefa Capuyan100% (1)
- KD 3.1 Offers and Suggestions: B. You ShouldДокумент5 страницKD 3.1 Offers and Suggestions: B. You ShouldHanna Nur MeidanaОценок пока нет
- Family Values LessonДокумент5 страницFamily Values LessonМария СинельниковаОценок пока нет
- Placenta Accreta ReportДокумент13 страницPlacenta Accreta ReportAnaОценок пока нет
- Sociology of Gender SyllabusДокумент8 страницSociology of Gender SyllabusWendy M. Christensen, Ph.D.Оценок пока нет
- Gynecology Enhancement: Maribee T. Espiritu, RN, MDДокумент178 страницGynecology Enhancement: Maribee T. Espiritu, RN, MDmaribeeОценок пока нет
- Global Report On Preterm Birth and StillbirthДокумент37 страницGlobal Report On Preterm Birth and StillbirthAbdullah ShiddiqОценок пока нет
- Practice Test 1 E11 1.2Документ2 страницыPractice Test 1 E11 1.2Hàn Bích DiệpОценок пока нет
- Berita Acara Minggu Ke 1Документ5 страницBerita Acara Minggu Ke 1Hidaya UlyaaОценок пока нет
- Quiz 9 Human Reproduction Pregnancy Menstruation GraphsДокумент4 страницыQuiz 9 Human Reproduction Pregnancy Menstruation GraphsAnonymous Azxx3Kp9Оценок пока нет
- The anatomy of bovine reproductive systemsДокумент26 страницThe anatomy of bovine reproductive systemsDivya Thuruthiyil RamachandranОценок пока нет
- SOAL BAHASA INGGRIS TENTANG MENARCHEДокумент2 страницыSOAL BAHASA INGGRIS TENTANG MENARCHENADIAОценок пока нет
- PROMДокумент21 страницаPROMJanelle Lois EscolanoОценок пока нет
- Gynecological Operation and Nursing ManagementДокумент29 страницGynecological Operation and Nursing Managementhawra alsaadОценок пока нет
- Women's Sexual Arousal Is Associated With Consistency of Orgasm But Not Other Sexual BehaviorДокумент10 страницWomen's Sexual Arousal Is Associated With Consistency of Orgasm But Not Other Sexual BehaviorAnonymous dh9lQyhsОценок пока нет
- Activity 1: Can You Justify Me?: Hormone Yes No ReasonДокумент2 страницыActivity 1: Can You Justify Me?: Hormone Yes No ReasonMa Rijubelyn Macaranas CapinpinОценок пока нет
- Family Tree and History BadonДокумент2 страницыFamily Tree and History BadonAlter BadonОценок пока нет
- 1-Evidence Based Midwifery CareДокумент11 страниц1-Evidence Based Midwifery Caresana naazОценок пока нет
- DAFTAR PUSTAKA-Azmi Indria Larasati-G1A019047-Skripsi-2023Документ4 страницыDAFTAR PUSTAKA-Azmi Indria Larasati-G1A019047-Skripsi-2023Azmi LarasatiОценок пока нет
- Woodson Family Probate Records PDFДокумент92 страницыWoodson Family Probate Records PDFBrian SheffeyОценок пока нет
- Revised ResearchДокумент14 страницRevised ResearchAlynna ValbuenaОценок пока нет
- Male and Female Reproductive Organs GuideДокумент2 страницыMale and Female Reproductive Organs GuidePink EaintОценок пока нет
- Stages of Labor: Definition, Signs, and OnsetДокумент73 страницыStages of Labor: Definition, Signs, and OnsetBharat ThapaОценок пока нет
- APH Types Causes ManagementДокумент13 страницAPH Types Causes ManagementdanielОценок пока нет
- Postterm Pregnancy RisksДокумент60 страницPostterm Pregnancy RisksArtika MayandaОценок пока нет
- 1117Документ5 страниц1117Melvin WijayaОценок пока нет
- Diagnostic Test in High Risk PregnancyДокумент36 страницDiagnostic Test in High Risk PregnancyRod Reynon BorceОценок пока нет
- Coital Alignment TechniqueДокумент2 страницыCoital Alignment Techniquenathan50% (6)
- Philippine AIDS Prevention Act ExplainedДокумент9 страницPhilippine AIDS Prevention Act ExplainedIrving Kelly B. PinedaОценок пока нет
- Dysmenorrhoea (Kashtartava) : An Ayurvedic Perspective: January 2015Документ4 страницыDysmenorrhoea (Kashtartava) : An Ayurvedic Perspective: January 2015sastalОценок пока нет