Академический Документы
Профессиональный Документы
Культура Документы
123 OpsAssessment (MPHCA08-09)
Загружено:
Sutikshna MishraИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
123 OpsAssessment (MPHCA08-09)
Загружено:
Sutikshna MishraАвторское право:
Доступные форматы
MISSISSIPPI PRIMARY HEALTH CARE ASSOCIATION
CONDUCTING AN OPERATIONS ASSESSMENT
Presented by: Michael R. Taylor, Precision Resources, Inc. MRTPRI@aol.com
SESSION GOAL
Share tactics that equip attendees to evaluate the effectiveness of their health centers operations and develop resulting plans for improvement
SESSION OVERVIEW
Hypothesize Assessment Objective(s) Analyze Relevant Information/Data Refine Assessment Objectives
Observations - What to Look for
Document Outcomes
Develop Implementation Plan
HYPOTHESIZE ASSESSMENT OBJECTIVES (SCHEDULING)
EFFECTS
Reports that staff is not helpful/courteous
POTENTIAL CAUSES
Individuals demeanor is incompatible with job requirements Individuals customer service training/ experience is inadequate
Increased volume of walk-in patients
Process is so cumbersome that it deters patients from booking appointments Insufficient phone lines cause unacceptably long hang/hold times Insufficient number of staff who book appointments
Too many patients arrive for their appointment unprepared/late
Patients are noncompliant Scheduler(s) are not conveying critical information (e.g., payment, insurance, referrals, underlying logic for scheduled time)
HYPOTHESIZE ASSESSMENT OBJECTIVES (REGISTRATION/DISCHARGE)
EFFECTS
Reports that staff is not helpful/courteous
POTENTIAL CAUSES
Individuals demeanor is incompatible with job requirements Individuals customer service experience is inadequate training/
Increased volume of denied claims because Staff dont verify coverage before each patients are not enrolled occasion of service Staff verifies coverage for current plans but dont update patient information in practice management system Less than acceptable cash collections Patients are noncompliant or unprepared Staff dont request payment routinely Staff dont know when deductibles and or co-payments apply
HYPOTHESIZE ASSESSMENT OBJECTIVES (PROVIDER VISIT)
EFFECTS POTENTIAL CAUSES
An inordinate number of Encounter Forms Providers are retaining Encounter Forms are unavailable for daily charge entry, and/or placing them in health records thus billing is decreased/delayed Encounter Forms disappear after being given to patients to return to the Registration Desk for discharge Payment is denied for a large volume of Provider coding is haphazard and training claims because diagnostic and procedure might be required codes are inconsistent Provider productivity acceptable is less than Nurses/Medical Assistants dont prepare exam rooms between patient visits Visits are prolonged because Providers attempt to address all patient conditions during one visit
HYPOTHESIZE ASSESSMENT OBJECTIVES (CHARGE CAPTURING)
EFFECTS POTENTIAL CAUSES
The amount and value of booked charges is All Encounter Form charges are not being low given the average number of monthly entered into the practice management patient visits system There is no daily reconciliation process or internal control measure that ensures appropriate charge entry/capturing
Charges havent been increased in five years The Encounter Form hasnt been updated in three years and, therefore, excludes new, high demand services
HYPOTHESIZE ASSESSMENT OBJECTIVES (BILLING/COLLECTIONS)
EFFECTS
Payment for an unacceptable number of claims is pended/denied because submitted patient information is incorrect inconsistent with payers data bases
POTENTIAL CAUSES
Registration staff dont verify patient information and/or ensure that it is accurately entered in the practice management system on each occasion of service
There is no internal control process that periodically checks the accuracy of claims before they are submitted
There is growing backlog of bills that No staff is available to research, correct require research and correction before the and resubmit old claims resubmission deadline There is insufficient oversight to ensure that staff correct and resubmit pended/denied claims in the prescribed time frame
NOW ITS YOUR TURN Take about 15 minutes
Think about your health centers operations
Identify two functional areas where youre fairly certain that improvement is warranted
Jot down one or two effects of each shortcoming
Then list what you think the potential causes are
The point is encourage you to think critically and in detail about how your health center functions
HYPOTHESIZE ASSESSMENT OBJECTIVES ( )
EFFECTS POTENTIAL CAUSES
HYPOTHESIZE ASSESSMENT OBJECTIVES ( )
EFFECTS POTENTIAL CAUSES
NOW ITS YOUR TURN
SHARE!
ASSESSMENT OBJECTIVES Cumulative CAUSES:
Are based, in many cases, on yet unsubstantiated perceptions and/or anecdotal information
Highlight where substantiating information/data might be needed Dont necessarily represent root causes BUT serve as a foundation to define initial assessment objectives and areas of focus
ANALYZE RELEVANT INFORMATION/DATA
Distinguish root causes from symptoms
Identify and analyze information/data necessary to substantiate/refute potential causes, and refine objectives and focus
Patient complaints Satisfaction survey results Call volume Encounter Forms
Remittance Advices
Encounter and patient volume data Financial management reports (e.g., financial statements, aged A/R by payer
ANALYZE RELEVANT INFORMATION/DATA
This is an ideal time to evaluate the adequacy of management information, and the capability and configuration of your practice management system
Do reports provide sufficient detail to substantiate or refute suspected causes? Are needed reports available/easily produced? Does the frequency of report production permit appropriate monitoring? Whos responsible for reviewing what reports and are they aware and held accountable for those responsibilities?
Create an information dashboard to monitor key operating functions on an ongoing basis
REFINE ASSESSMENT OBJECTIVES
Use analytical outcomes to:
Confirm, refute and refine assessment objectives
Inform the types of activities required to substantiate potential causes and conclude improvement initiatives
What data should you analyze What operations functions should you observe
OBSERVATIONS - WHAT TO LOOK FOR (WAITING ROOM)
Signage should communicate:
Patient rights and responsibilities
Payment expected and due at the time of service Walk-ins will be seen in their order of arrival but only as permitted by appointed patients Patients arriving more than 15 minutes late for appointments will be treated as walk-ins
Hours of operation The availability of discounted fees for qualifying patients and how to apply Acceptable forms of payment Participating health plans
Registration instructions
OBSERVATIONS - WHAT TO LOOK FOR (WAITING ROOM)
Cycle Time Durations
Arrival to Registration
Registration to Retrieval Retrieval to Provider Entry Provider Entry to Exam Completion Exam Completion to Discharge
Facilities
Attractive, functional, safe and clean Adequate, comfortable seating
OBSERVATIONS - WHAT TO LOOK FOR (WAITING ROOM)
Front Desk
How many and to whom do they report
Staff interactions with patients (e.g., welcoming, courteous, observant)
Appearance of order or chaos
Frequency and pervasiveness of interruptions (e.g., telephone calls , other staff members, visitors) and unrelated functions Frequency, timing and content of payment requests
Patient reactions to payment requests
OBSERVATIONS - WHAT TO LOOK FOR (BEHIND THE FRONT DESK)
Staff interactions with patients (e.g., welcoming, courteous, observant) Appearance of order or chaos (e.g., designated locations for key tools and resources) Frequency and intrusiveness of interruptions
Telephone (related vs. unrelated) Other staff members (appropriate vs. inappropriate) Visitors (vendors, sales people, deliveries)
OBSERVATIONS - WHAT TO LOOK FOR (BEHIND THE FRONT DESK)
Payment requests
Are requests made routinely When is payment requested How are requests made Do staff know when co-payments and deductibles apply and the amount to request
Are patient accounts checked for previous balances
Patient reactions to payment requests
Do requests seem expected Are patients prepared to pay
OBSERVATIONS - WHAT TO LOOK FOR (BEHIND THE FRONT DESK)
Patient registration
Is process confidential
Are identification and insurance cards copied Is copy machine proximate and functioning
Insurance verification
Do staff inquire re secondary payers Is verification process quick, easy, reliable and accessible Do staff check to ensure that verified plan information is consistent with patients account Are notations made when coverage is verified
OBSERVATIONS - WHAT TO LOOK FOR (BEHIND THE FRONT DESK)
Encounter Forms
Are they numbered to permit subsequent reconciliation
Who handles them, before and after provider visit
Health Records
Are they available and complete for appointed patients
Can they retrieved quickly for established walk-in patients
Is production relatively easy for new walk-in patients
OBSERVATIONS - WHAT TO LOOK FOR (BEHIND THE FRONT DESK)
Health Records
-Is access to the central storage restricted to approved staff -Are Out Guides used and completed sufficiently to identify the location of pulled charts
HEALTH RECORDS
-Do most Out Guides indicate that charts were pulled fairly recently
-Are records organized reasonably to locate key ARE THEY AVAILABLE AND documents (e.g., most recent H&P, progress notes, COMPLETE etc) FOR APPOINTED medications list, PATIENTS
OBSERVATIONS - WHAT TO LOOK FOR (BEHIND THE FRONT DESK)
Financial Counseling
Are uninsured patients routinely referred by registration staff
Do uninsured, appointed patients usually bring income documentation What do staff do when/if patients report no income
Do staff evaluate patient eligibility for public insurance programs, either first or simultaneous with center discounts
OBSERVATIONS - WHAT TO LOOK FOR (BEHIND THE FRONT DESK)
Financial Counseling
Is there a policy that requires periodic recertification
Is there a mechanism to alert staff when recertification is required Does policy require patients to pay full charges prior to eligibility determination or qualification for center discounts
OBSERVATIONS - WHAT TO LOOK FOR (BEHIND THE FRONT DESK)
Discharge/Charge Entry
Do staff conduct a daily reconciliation process that accounts for: All Provider-completed Encounter Forms Collected cash and credit card receipts What does staff do if Encounter Forms are missing
How soon after service are charges entered into the practice management system for billing and to determine patient liability Is an another request made for payment Are patients reminded again about any previous balance
OBSERVATIONS - WHAT TO LOOK FOR (SCHEDULING)
Communications Content
Who and how many staff perform the scheduling function
How do schedulers know the amount of time that should be to assigned to each visit Is staff courteous, helpful and knowledgeable On average, how many times does the phone ring before being answered
On average, how long and how frequently are patients placed on hold
Are patient accounts checked for previous balances
OBSERVATIONS - WHAT TO LOOK FOR (SCHEDULING)
Communications Content
Are schedulers equipped with a current list of health plans that the center accepts including copays, deductibles, referral/ preauthorization requirements, non-covered health center services
Are patients informed that payment is expected and will be requested at the time of service
Do staff communicate the minimum amount patients should be prepared to pay Are uninsured patients informed that they must provide proof of income to qualify for discounted fees
OBSERVATIONS - WHAT TO LOOK FOR (SCHEDULING)
Communications Consistency
Are patients instructed to bring proof of identification and their insurance card, if any Are patients informed that they will be treated as a walk-in if they are more than 15 minutes late Do staff know when co-payments and deductibles apply and theirs amounts What tools are used to ensure consistent, comprehensive communications with patients (script, checklist, etc) Are schedulers equipped with a current list of health center charges
OBSERVATIONS - WHAT TO LOOK FOR (PATIENT VISITS)
Patient Visits
Are provider productivity standards communicated/reflected in employment agreements
Do provider productivity levels meet acceptable norms (If not, why
What percentage of provider time is spent off-site (e.g., attending inpatients, traveling between sites)
Do providers prolong patient visits because they attempt to treat multiple conditions during a single visit Do all providers use the same scheduling template
Do providers submit legibly completed Encounter Forms in a timel manner
OBSERVATIONS - WHAT TO LOOK FOR (CODING)
Documentation and Coding
Do providers complete Encounter Forms appropriately and on a consistent basis Who performs coding functions, aside from services listed on the Encounter Form Is the Encounter Form updated frequently enough to ensure that it includes current, commonly used procedure codes Do record notes seem to support selected codes Does the health center either employ or engage a professional Coder who periodically reviews provider documentation and coding practices
OBSERVATIONS - WHAT TO LOOK FOR (BILLING)
Timely, Accurate Submissions
Are bills sent out/submitted within an acceptable time from the date of service
Are claims submitted electronically, wherever possible Are sample claims spot checked periodically to identify developing problems
OBSERVATIONS - WHAT TO LOOK FOR (BILLING)
Claims Backlogs
Is there a backlog of unbilled claims
Is there a backlog of previously denied or pended claims that require correction and resubmission
How significant is/are the backlog(s)
Can claims values be sorted by dates of service and by payer Is staff familiar with each payers claims submission deadline Is there an adequate, ongoing effort to clear any backlog(s)
OBSERVATIONS - WHAT TO LOOK FOR (PAYMENT POSTING & DEPOSITS)
Payment Posting Are payments posted to patient accounts within a reasonable time of receipt Is posting done manually or electronically Is electronic posting possible
Are denial reasons/codes posted to patient accounts
Are prevailing denial reasons summarized by payer in a periodic management report
OBSERVATIONS - WHAT TO LOOK FOR (COLLECTIONS)
Payment Deposits
Is EFT in place, wherever possible Are deposits made within a specified time of receipt Who makes deposits How are timely deposits ensured
Remittance Advices (RAs)
Who reviews RAs Are RAs reviewed within a specified time after receipt What actions are taken when and by whom on pended and denied claims Are and how are prevailing reasons for denied claims communicated to other staff
OBSERVATIONS - WHAT TO LOOK FOR (COLLECTIONS)
Patient Payments
Have/can historical cash collections be determined by site as a basis to establish a cash collections target Are cash collections reasonable given encounter volume and payer mix
ITS YOUR TURN AGAIN!
Go back to the exercise you completed on pages 10 and 11
What data would you analyze and/or operating functions would you observe to substantiate the POTENTIAL CAUSES you defined?
DOCUMENT PROCESS & OUTCOMES
A written assessment report should document:
Defined objectives
Activities (the process that was followed) Conclusions, as supported by analyses and/or observations Recommendations for improvement
Share draft report with entire management team to gain additional insight, buy in and refine recommendations
DOCUMENT PROCESS & OUTCOMES
Documenting Outcomes will:
Help you digest and consider the implications of assessment findings
Highlight the need for additional information and/or further investigation Assist in quantifying both the value of corrective actions and the cost of implementing them Establish a foundation to develop an implementation plan
DEVELOP IMPLEMENTATION PLAN
Segment recommendations between
Easy Fixes: relatively quick, inexpensive and easily implemented actions that will yield near term results
AND Longer Term Solutions: more complex initiatives that will require a significant financial and/or staff investment, inter departmental coordination and cooperation, and/or major change to organizational philosophy and procedures
DEVELOP IMPLEMENTATION PLAN
Should include:
Defined objective(s) Sequential implementation tasks Corresponding responsible party(ies) Benchmark(s) that will be used to measure effectiveness Implementation time frame Required financial investment and likely return, as appropriate
SUMMARY
A well conceived and executed operations assessment should yield the intelligence youll need to:
Improve patient satisfaction
Increase patient throughput
Enhance staff productivity Increase quality of care Improve collections and overall financial performance
SUMMARY
To achieve results, however, youll likely have to:
Revise policies and procedures Update staff job descriptions
Re-train staff
Modify information systems Educate patients
Monitor performance
Measure impact
QUESTIONS
Вам также может понравиться
- Trimmed JSW Lakshya 1.0Документ27 страницTrimmed JSW Lakshya 1.0Sutikshna MishraОценок пока нет
- Commission Master For Insurance Products: Insurance Provider: ICICI Prudential Life Insurance Co. LTDДокумент5 страницCommission Master For Insurance Products: Insurance Provider: ICICI Prudential Life Insurance Co. LTDSutikshna MishraОценок пока нет
- Writing Instructional ObjectivesДокумент35 страницWriting Instructional ObjectivesSutikshna MishraОценок пока нет
- Personal Accident: An Investment To Protect Your Family's FutureДокумент4 страницыPersonal Accident: An Investment To Protect Your Family's FutureSutikshna MishraОценок пока нет
- Leader As Coach1Документ3 страницыLeader As Coach1Sutikshna MishraОценок пока нет
- Mock Test QuestionsДокумент15 страницMock Test QuestionsSutikshna MishraОценок пока нет
- Anandam JoyДокумент13 страницAnandam JoySutikshna MishraОценок пока нет
- Interesting Facts in SalesДокумент1 страницаInteresting Facts in SalesSutikshna MishraОценок пока нет
- AO SmithДокумент10 страницAO SmithSutikshna MishraОценок пока нет
- CV - Pulkit Shukla - Doc-1Документ8 страницCV - Pulkit Shukla - Doc-1Sutikshna MishraОценок пока нет
- AO SmithДокумент10 страницAO SmithSutikshna MishraОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
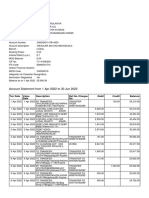
- Account Statement From 1 Apr 2022 To 30 Jun 2022: TXN Date Value Date Description Ref No./Cheque No. Debit Credit BalanceДокумент10 страницAccount Statement From 1 Apr 2022 To 30 Jun 2022: TXN Date Value Date Description Ref No./Cheque No. Debit Credit BalanceParveen SainiОценок пока нет
- Qazi Mohsin Ali: Career ObjectiveДокумент4 страницыQazi Mohsin Ali: Career ObjectiveSamia KhalidОценок пока нет
- Hostel ManualДокумент30 страницHostel ManualpupegufОценок пока нет
- Uniform Loan Delivery Data - Set FaqsДокумент4 страницыUniform Loan Delivery Data - Set FaqsraghuОценок пока нет
- Nature of PostsДокумент13 страницNature of PostsSagargn SagarОценок пока нет
- Banking in India For WbcsДокумент29 страницBanking in India For WbcsSubhasis MaityОценок пока нет
- UK Financial Regulation Ed23-5 PDFДокумент298 страницUK Financial Regulation Ed23-5 PDFVincenzo Somma100% (2)
- Financial Services Project Manager CVДокумент2 страницыFinancial Services Project Manager CVMike KelleyОценок пока нет
- Project On Mutual FundsДокумент86 страницProject On Mutual Fundsmohindrudinit88% (33)
- SOREV Income Approach DiagnosticДокумент4 страницыSOREV Income Approach DiagnosticReyn شكرا100% (1)
- Bajaj Finserv (BAFINS) : Finance Momentum Strong Life Picks UpДокумент12 страницBajaj Finserv (BAFINS) : Finance Momentum Strong Life Picks Uparun_algoОценок пока нет
- Maths ProjectДокумент15 страницMaths Projecttmbcreditdummy50% (2)
- Retail Loan Rates Comparision Chart PDFДокумент3 страницыRetail Loan Rates Comparision Chart PDF9778486995Оценок пока нет
- Collaborative Consumption With Rachel BotsmanДокумент28 страницCollaborative Consumption With Rachel BotsmanSeokwon Yang100% (1)
- Madoff's American Express Corporate Card StatementДокумент30 страницMadoff's American Express Corporate Card StatementInvestor Protection100% (3)
- Barkatullah Vishwavidyalaya Migration Cert - Format FilledupДокумент5 страницBarkatullah Vishwavidyalaya Migration Cert - Format FilledupRojukurthi SudhakarОценок пока нет
- Chap 002 NotesДокумент43 страницыChap 002 NotessamiullahaslamОценок пока нет
- Chapter 13 The Human Resources Management and Payroll CycleДокумент67 страницChapter 13 The Human Resources Management and Payroll CycleislamelshahatОценок пока нет
- Code Movement Sub Movement Code Number SourceДокумент44 страницыCode Movement Sub Movement Code Number SourceSanath SuvarnaОценок пока нет
- Shwethacoffee11 PDFДокумент6 страницShwethacoffee11 PDFabhilash eshwarappaОценок пока нет
- Xtreme Dance January Newsletter 2012Документ1 страницаXtreme Dance January Newsletter 2012incontroltechОценок пока нет
- BillSTMT 4588260000514267Документ3 страницыBillSTMT 4588260000514267Fahad AhmedОценок пока нет
- A Study On Customers Satisfaction-1102-With-cover-page-V2 Ex ProjectДокумент16 страницA Study On Customers Satisfaction-1102-With-cover-page-V2 Ex ProjectFelix ChristoferОценок пока нет
- Loans User Manual PDFДокумент600 страницLoans User Manual PDFdevarchitОценок пока нет
- Case Study - 6: TITLE: Corporate Failure (Money Laundering)Документ7 страницCase Study - 6: TITLE: Corporate Failure (Money Laundering)KanakaMaha LakshmiОценок пока нет
- Case 11 A LBP V RiveraДокумент8 страницCase 11 A LBP V RiveraNathalie YapОценок пока нет
- Internship Report Format For UIMSДокумент17 страницInternship Report Format For UIMSasimkhan2014Оценок пока нет
- Payment Process Request Status ReportДокумент1 страницаPayment Process Request Status ReportNishant RanaОценок пока нет
- Chinese Busssines ReviewДокумент136 страницChinese Busssines Reviewamir hamzahОценок пока нет
- Forms of Registration Under Contract Labour Act 1970 PDFДокумент7 страницForms of Registration Under Contract Labour Act 1970 PDFGlendaОценок пока нет